Case 1: A patchy lichenoid infiltrate with epidermotropism can be appreciated at low power.
At higher power, one can see the atypical lymphocytes at the dermal-epidermal junction and migrating up into the epidermis. Although so-called cerebriform lymphocytes may be seen in some cases, the lymphocytes just look normal in many cases.
Cleaved irregular (perhaps even cerebriform) lymphoid cells with many mitotic figures. This is a more advanced lesion, possibly even progressing toward Sezary syndrome.
Case 3: This image shows a very robust lichenoid infiltrate. Epidermotropism is visible even at this low power. There is also a hint of papillary dermal fibrosis.
A higher power view of the atypical clonal CD4 lymphocytes in the dermis.
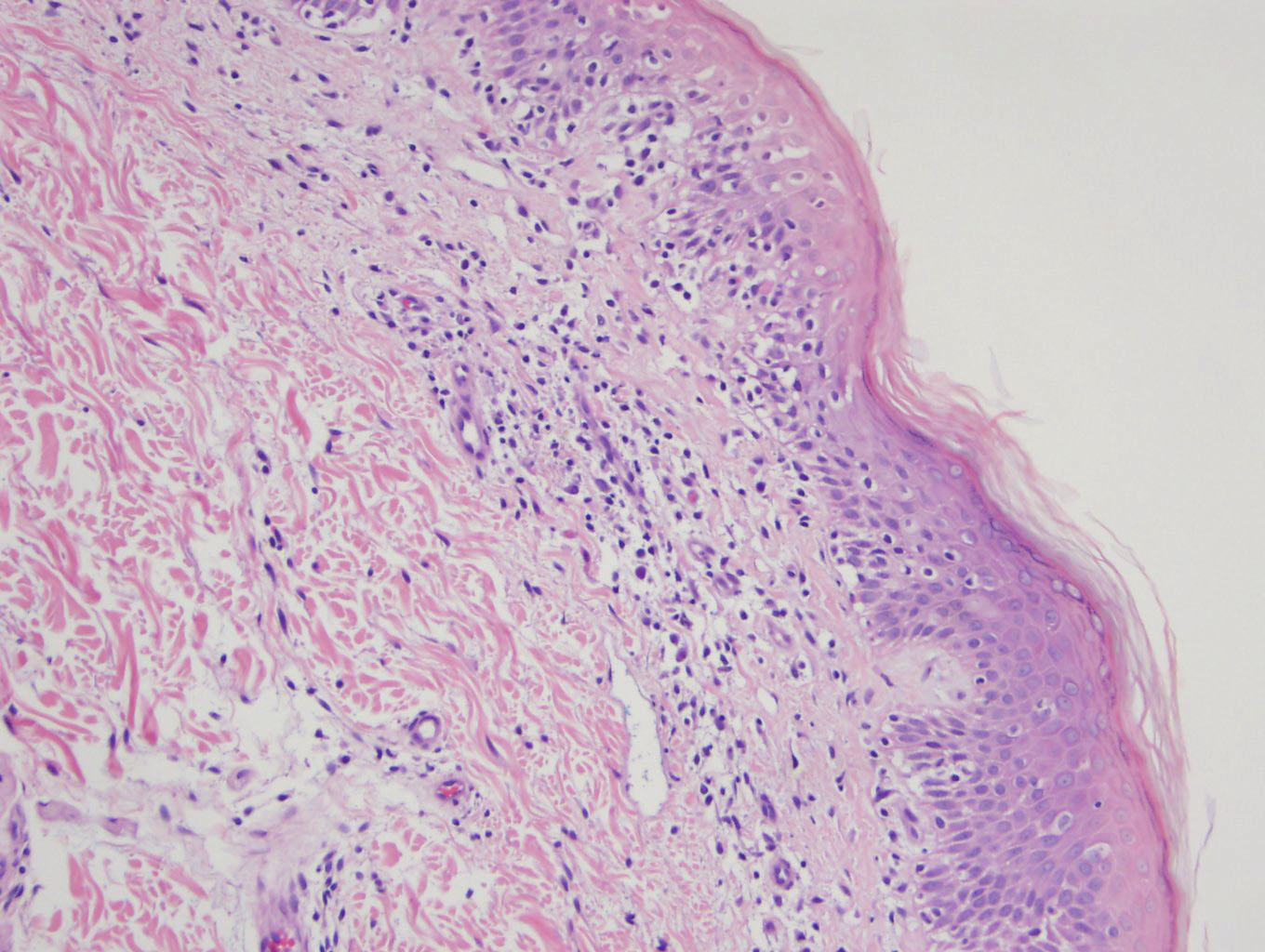
Case 4: This particular case has a smattering of eosinophils. Papillary dermal fibrosis (wiry collagen) can be appreciated here.
On high power, eosinophils are mixed in with the atypical lymphocytes, which have irregular nuclear contours. Early diagnosis of mycosis fungoides is sometimes challenging, as the pathologic features of inflammatory dermatoses and MF may show significant overlap. One helpful criterion to distinguish early MF (patch stage) from dermatitis is the presence of eosinophils.
Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL), comprising approximately 44% of cases. In the past, MF was considered synonymous with CTCL, however, many other types of cutaneous T-cell lymphomas (e.g. lymphomatoid papulosis, subcutaneous panniculiticlike T-cell lymphoma) have been discovered and classified into the WHO-EORTC (European Organization for Research and Treatment of Cancer) system.
Mycosis fungoides was thus named because of the large fungating masses (resembling mushrooms) growing on the patient's skin. There are three stages of MF: (1) eczematous patch stage: centered on the hip and buttocks, this stage can last for years; (2) papulosquamous plaques; eventually, the patches merge to plaques (3) tumor nodules - fungating tumor nodules are seen.
Some cases of MF progress to the Sezary syndrome, considering the advanced form of MF in which the patient has generalized erythroderma, lymphoadenopathy and greater than 1000 Sezary cells per cubic millimeter of periphal blood.
MF cells are clonal CD4+ memory T cells (CD45RO+) that normally patrol the skin. This malignant clone may have aberrant loss of T-cell antigens such as CD2, CD5 or CD7.
Microscopically, there is a lichenoid or patchy lichenoid infiltrate of lymphocytes. Sometimes, the atypical lymphocytes may exhibit cerebriform nuclei, but often times, they use appear as normal lymphocytes. Plasma cells and eosinophils may be seen as well. Another characteristic finding is epidermotropism (migration of lymphocytes to the epidermis) creating "punched-out" white spaces in the epidermis. Pautrier microabcesses (composed of lymphocytes in epidermis) are also very common (Rapini).
~ 1000 new cases of mycosis fungoides occur per year in the US. It is more frequent in men (M:F ratio of 2:1), and the mean age at presentation is 50. However, the condition has been diagnosed in children and adolescents (Pinter-Brown).
For disease limited to the skin, skin-directed therapies (nitrogen mustard, steroid) is preferred, while patients with advanced-stage disease with significant nodal, visceral, or blood involvement are generally approached with biologic-response modifiers, denileukin diftitox, and histone deacetylase inhibitors before trying chemotherapy (Wilcox).
The majority of those with mycosis fungoides typically have an indolent disease course, although a minority undergo a process of large-cell transformation, which often heralds more aggressive disease and shortened survival.
Pinter-Brown LC. Cutaneous T-Cell Lymphoma Overview of CTCL. eMedicine. Last updated on May 17th 2011. Available at: emedicine.medscape.com/article/209091-overview
Rapini RP. Practical Dermatopathology. Philadelphia, PA: Elsevier; 2005: 309-310.
Wilcox RA. Cutaneous T-cell lymphoma: 2011 update on diagnosis, risk-stratification, and management.
Am J Hematol. 2011 Nov;86(11):928-48.
