
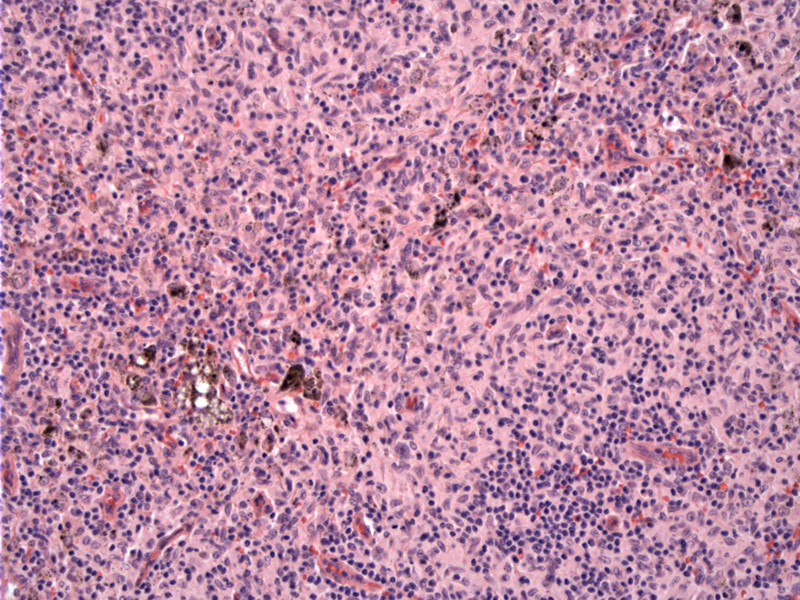
Expansion of the paracortex by Langerhans cells, interdigitating dentritic cells, histiocytes and small lymphocytes can be appreciated. The melanin pigments are usually ingested by the histiocytes.
Dermatopathic lymphadenitis occurs in lymph nodes that drain areas of disrupted, inflamed, or neoplastic skin (e.g. psoriasis, skin infectino, mycosis fungoides). When skin antigens are presented by interdigitating dendritic cells (IDC), the T-cells proliferative.
On low power, the lymph node architecture is preserved, but the cortex may be compressed toward the capsule due to marked expansion of pale confluent areas in the paracortex. The expansion may be diffuse or nodular, and there is a proliferation of Langerhans cells and interdigitating cells, which have similar morphologies (intermediate nuclear size, fine chromatin, irregular nuclear membranes and a "coffee-bean" shape). Histiocytes (with ingested melanin) and a variable number of plasma cells, eosinophils and small lymphocytes may be present (Weiss, Iaochim).
The prominent presence of Langerhans cells can be highlighted by CD1a and S-100. The interdigitating cells are CD1a negative and S-100 positive and macrophages are CD168 positive.
The main differential diagnosis would be lymph nodes involved by mycosis fungoides, as these patients often have superimposed dermatopathic changes. If there is any suspicion, ordering a T-cell receptor gene rearrangement may be in order (Weiss).
Some patients may provide a history of pruritis and scratching, but in a minority of patients, there is no recollection of a skin lesion. The presentation is usually an isolated or generalized lymphadenopathy. Axillary and inguinal lymph nodes are most often affected and some patients may have eosinophilia in their peripheral blood (Iaochim).
→Key differential diagnosis is mycosis fungoides. This is complicated by the fact that lymph nodes involved by mycosis fungoides often have superimposed dermatopathic lymphadenitis.
Iaochim HL. Lymph node pathology, 4th ed. Philadelphia, PH: Lippincott, Williams and Wilkins; 2008: 226.
Weiss L. Lymph nodes: Illustrated Surgical Pathology New York, NY: Cambridge University Press; 2008: 45-7.