
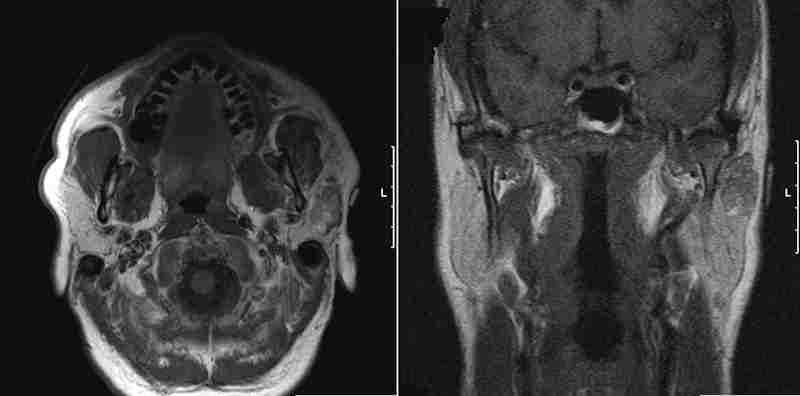
T1 MRI sequences in axial and coronal planes demonstrating a left sided parotid mass.
The intraoperative image shows a superficial lobe parotid mass with the facial nerve seen deep to the mass.
This intraoperative image shows an acinic cell cancer of the superficial lobe of the parotid gland which required dissection directly off of the facial nerve. Further resection was subsequently done deep to the facial nerve with preservation of this structure.
The resection specimen is fairly well demarcated and is encircled by benign parotid tissue.
Bisection shows a lesion with cystic change and hemorrhage which extruded serosanginous fluid. The lack of a capsule or well-delineated edge is compatible with a malignant tumor.
Bisected view of another acinic cell carcinoma which demonstrates a solid growth pattern with a more well defined border.
Although initially confusing, this image demonstrates several features common to acinic cell carcinomas. (1) a pseudocystic cavity containing discohesive tumors cell, hemorrhage and hemosiderin-laden macrophages representing cystic degeneration, (2) cytoplasmic vacuolization, and (3) microcysts.
Acinic cell carcinomas are generally very cellular tumors, with very little intervening stroma (except for fibrous bands between tumor nodules if the tumor is multinodular). In this image, there is a solid sheet of tumor cells punctuated by microcysts (not be be confused with larger cystic areas, also a feature of this tumor). Solid, microcystic, glandular patterns are common growth patterns for this tumor. Notice that this lesional cells resemble serous acinar cells of salivary glands, and hence the name "acinic cell carcinoma". In contrast to non-neoplastic acinar cells, the cells are polygonal instead of the normal triangular shape with greater size variability, and there is increased nuclear hyperchromasia.3
Acinic cell carcinomas often undergo ischemia and infarction. Thus, cystic degeneration and secondary hemorrhage can often be found grossly (seen in the bisected gross photo), and microscopically. This image demonstrates cystic areas contain hemorrhage and hemosiderin-laden macrophages.
This image demonstrates acinar cells with focal mild atypia. There is some variation in cell size and nuclear pleomorphism, but the degree of atypia is not severe.
There is a partial capsule around the tumor, separating the tumor from the normal parotid tissue. Note that the tumor has invaded into the capsule. Other areas of this tumor (not shown here) demonstrated frank invasion of adipose tissue by malignant acinar cells.
Focal areas shows cytoplasmic vacuolization, a feature very characteristic of acinic cell carcinoma. Note the presence of microcysts; the cells do not oriented around the microcystic lumens, which distinguishes these cystic spaces from true glandular formation.
The pre-operative FNA of the parotid mass showed loosely cohesive sheets of cells with clear cytoplasm and round nuclei, but in an irregular arrangement.
Diff quick stain of the parotid shows cells resembling acinar cells but with larger and more (multiple) nuclei. There is a lack of an acinar arrangement, which should be seen in a benign salivary gland. Mitoses and significant nuclear atypia is not seen. Such features all taken together should lead one to the diagnosis of acinar cell carcinoma.
The cell block contains many cells with an overall similar appearance and resemblance to acinar cells.
This is a different case of an acinic cell with clear cell features, located near the tongue in the oral cavity. Note that acinic tumor cells can have a wide range of morphologies, ranging from acinic cells, to intercalated duct cells, non-specific glandular cells, vacuolated cells and clear cells.
WHO classification of salivary gland malignancies.
Acinic cell carcinoma is an uncommon malignancy of the progenitor reserve cells of the terminal tubules and intercalated ducts of salivary tissue and comprises about 5-10% of salivary malignancies1 . In general, this malignancy follows a less aggressive course than some higher grade malignancies of the salivary tissue, in fact until the 1950's, it was generally considered a benign disease.
Patients usually present with a painless enlarging mass. There is not sex strong predilection, and acinic cell carcinoma affects middle age or older individuals(median age 52yrs.). About 85% of acinic cell cancers present in the parotid gland2 , with the remainder spread throughout the other salivary tissue in the head and neck. The standard TNM staging system is used to stratify individuals diagnosed with this disease.
Surgery is the primary treatment with complete excision being associated with fewer local recurrences. Radiation therapy is used as adjuvant treatment in cases with incomplete excision or evidence of regional metastasis.
Due to the wide range of morphologies and rarity of the tumor, histologic grading to predict prognosis had not been developed and consistently applied. Several pathology texts make cursory mention of morphologic features associated with a more aggressive tumor.3,4 However, a recent study by Gomez et al clarified criteria for high-grade tumor, defined as: high mitotic activity (greater than 2 mitoses per 10 HPF), focal areas of necrosis, pleomorphism, extracapsular extension and positive surgical margins. These features were associated with significant differences in overall survival, with the overall 5-year survival of 69% versus 100% (100% being cases without high-grade features).1
• Salivary Gland : Small Cell Carcinoma (of parotid)
1 Gomez DR, Katabi N, Zhung J, Wolden SL, Zelefsky MJ, Kraus DH, Shah JP, Wong RJ, Ghossein RA, Lee NY. Clinical and pathologic prognostic features in acinic cell carcinoma of the parotid gland. Cancer. 2009 May 15;115(10):2128-37
2 Hoffman HT, Karnell LH, Robinson RA, Pinkston JA, Menck HR. National Cancer Data Base report on cancer of the head and neck: acinic cell carcinoma. Head Neck. 1999;21:297-309.
3 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 284-6.
4 Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004:891-2.