The WHO classification of ameloblastoma includes several different varieties.
Case 1: The follicular type of ameloblastoma shows small islands of cells and some with mild cystic dilation lined by more squamoid appearing cells.
The neoplastic epithelium forms discrete islands in a dense fibrous background.
Islands of ameloblastic epithelium with fingerlike projections are seen.
Peripheral pallisading may be focal (as seen here) or diffuse.
Case 2: In the plexiform type, the odontogenic epithelium is arranged in anatomosing cords separated by scant connective tissue.
In this variant, the peripheral pallisading is more evident and cells resembling stellate reticulum are evident within the epithelial cords.
Case 3: CT scan shows a 3 cm right mandibular mass.
The classic follicular pattern is well-demonstrated here with follicles composed of ameloblastic epithelium. Inside the follicles, a loose network of stellate cells are seen.
A more plexiform pattern is seen in this area. The neoplastic cells form interconnecting cords and the stroma is quite collagenous and dense, although not quite desmoplastic
More than one pattern is often encountered in an ameloblastoma as seen here. The top part of the image is plexiform/desmoplastic whereas the lower half of the image demonstrates an ill-defined follicles surrounded by a spindled stroma.
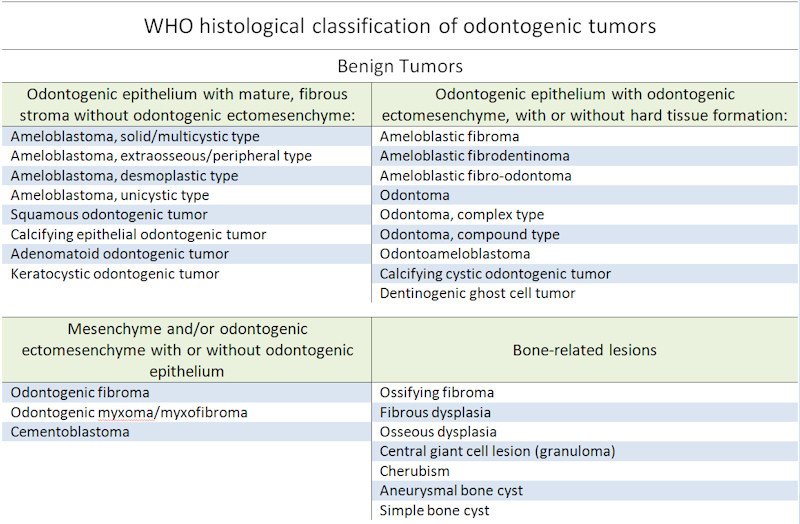
Ameloblastoma is the most common odontogenic tumor and arises from odontogenic (tooth-forming) epithelium. It is considered a benign slow-growing lesion, although it can be locally aggressive and recur. Rarely, these neoplasms can undergo malignant transformation into malignant ameloblastoma or ameloblastic carcinoma.
Ameloblastomas are divided into several subtypes: solid/multicystic, extraosseous/peripheral, desmoplastic and unicystic (Thompson). These variants have slightly different clinicopathologic features. For example, the unicystic subtype tends to occur at a younger age (2nd and 3rd decade), whereas the peripheral subtype occurs commonly occurs in the 5th decade. The unicystic subtype has a recurrence rate of 5-10% whereas the solid/multicystic subtype has a recurrence rate as high as 35% (Barnes).
The "conventional" ameloblastoma has a predominantly follicular or plexiform pattern. The cells forming the follicles are unique-appearing columnar cells whose nuclei are oriented opposite to the basement membrane. These cells are similar to the pre-ameloblasts seen in normal tooth development. The follicles may be cystically dilated and/or contain loosely arranged stellate cells (Fletcher). The plexiform pattern consists of interconnecting cords of epithelial cells.
Other variants include acanthomatous (squamous metaplasia within follicles), granular cell (granular cells within the follicles), desmoplastic (collagenous stroma compressing epithelial cords) and basaloid (islands of basaloid neoplastic cells).
Unicystic ameloblastoma should be recognized because both the surgical management and prognosis are significantly different from that of conventional ameloblastoma. Unicystic ameloblastomas arise in a younger age group (usually in their 20s) and tend to have a favorable prognosis with low recurrence, even after conservative surgery.
Ameloblastomas affect a wide age range (2nd to 6th decade), although the unicystic variant tends to arise in a younger population (2nd to 3rd decade). Presenting symptoms may include a slow-growing submucosal mass, loose teeth, and pain. The majority of intraosseous cases arise in the posterior mandible (Thompson).
Treatment for ameloblastoma is surgery, which varies from conservative treatment, such as enucleation and/or curettage, to wide resection. Because the probability of recurrence is high after conservative procedures, many recommend wide resection with 1 to 1.5 cm bony margins (Becelli; Carlson). Patients with positive margins who are not amenable to re-excision and those with incompletely resectable tumors may be considered for radiotherapy (Mendenhall).
Most clinicans feel that the solid/multicystic variant is a more locally aggressive lesion. These variants have a higher recurrence rate following less aggressive treatments such as enucleation or curettage.
Unicystic ameloblastomas have significant recurrence potential, but are thought to be less locally destructive than the solid or multicystic types. These lesions may respond to enucleation or curettage.
Finally, peripheral ameloblastomas, often encountered in the soft tissues of the gingiva, may have a different pathogenesis ofter respond well to local excision (Pogrel).
→Ameloblastoma may be central or peripheral. The central type arises within the jaw whereas the peripheral type arises in the gingiva without involvement of the underlying bone.
→There are numerous histologic subtypes such as plexiform, follicular, desmoplastic, basaloid, granular cell, acanthomatous and unicystic. The histologic subtype does not affect prognosis, however.
Thompson LDR, Wenig BM, eds. Diagnosis Pathology: Head and Neck. 1st Ed. Manitoba, Canada; Amirsys;2011; 6-32-7.
Becelli R, Carboni A, Cerulli G, et al. Mandibular ameloblastoma: analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofac Surg. 2002;13:395–400.
Carlson ER, Marx RE. The ameloblastoma: primary, curative surgical management. J Oral Maxillofac Surg. 2006;64:484–494.
Fernandes AM, Duarte EC, Pimenta FJ, et al. Odontogenic tumors: a study of 340 cases in a Brazilian population. J Oral Pathol Med. 2005;34:583–587.
Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Ameloblastoma. Am J Clin Oncol. 2007 Dec;30(6):645-8.
Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg. 2009 Aug;38(8):807-12.
Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86–99.