
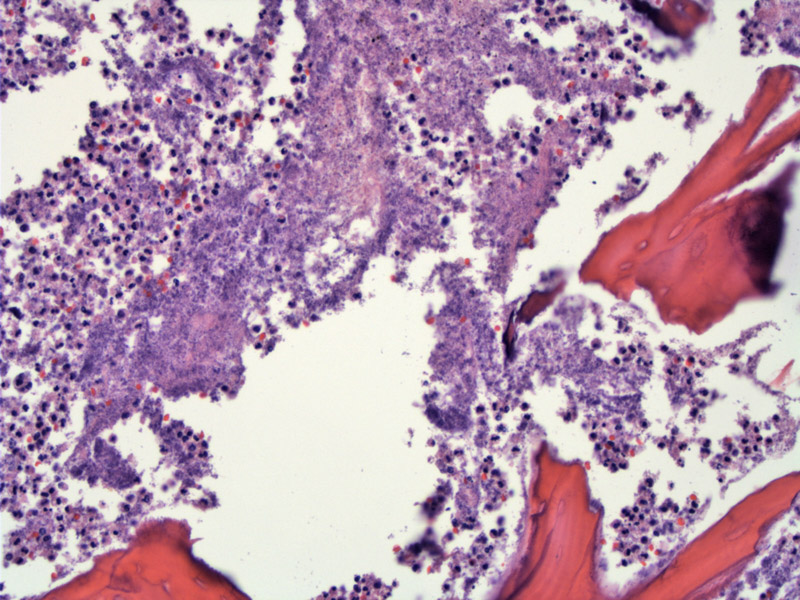
A key feature of acute osteomyelitis is necrotic bone (no viable osteocytes) surrounded by a neutrophilic infiltrate.
Bone fragment with scalloped edges and surrounded by neutrophilic debris.
Inter-trabecular serous fat atrophy is also characteristic. Again, the bone is necrotic.
Another case shows a scalloped margin to the bone along with a brisk neutrophilic infiltrate indicative of marked acute osteomyelitis.
Inflammation in bone is most likely due to infection, however, one must also consider other etiologies such as trauma, metabolic conditions such as gout and malignancy. There are two routes of infection: hematogenous or direct implantion.
Direct implantation of bacteria into bone can occur after puncture wounds, fractures or surgery. They are not uncommon complications of joint replacements.
Hematogenous osteomyelitis mostly affect children, and the preferential sites of infection are areas of rapid growth (growth plates of long bones such as the distal femur, proximal femur, proximal tibia, proximal humerus and distal radius). Interestingly, children have large caliber metaphyseal veins where blood flows more slowly, thus, placing them at a higher risk of thrombosis and seeding of microbes when bone tissue is injured.1 The culprit organism in children is usually Staphylococcus aureus, followed by Streptococcus pyogenes and Haemophilus influenzae. In debilitated adults, the most common organism is also Staphylococcus aureus, however, gram-negative bacteria and yeasts can be a cause in IV drug users.
Note that whereas the knee is the most common site of infection in children, the spine is most commonly affected in adults. In hospitalized patients on multiple antibiotics, Pseudomonas aeruginosa can enter the spine and cause spinal osteomyelitis. In diabetics with foot ulcers, the infections are often polymicrobial. In patients with sickle cell disease, Salmonella is often the causative organism and affects multiple sites. Granulomatous infection is most frequently caused by Mycobacterium tuberculosis, and TB in the spine is known as "Pott's disease".
Since the advent of antibiotics, the incidence of osteomyelitis has decreased dramatically and mostly now affects the elderly, immunocompromised persons such as diabetics or as a complication of trauma (surgery or fractures).1
Patients present with pain and tenderness around affected joint and may exhibit systemic symptoms of infection such as fever. In children, the presentation may mimic that of Ewing sarcoma (fever, increased sedimentation rate and leukocytosis).2
1 Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 261-2.
2 Silverberg SG. Silverberg's Principles and Practice of Surgical Pathology and Cytopathology. Philadelphia, PA: Elsevier; 2006:689-90.