
Endometriosis involving the GI tract is often situated in the serosa or muscularis propria and may elicit fibrous adhesions. Endometrial glands and stroma with associated hemosiderin deposition (not clearly visible here) clinch the diagnosis of endometriosis. The morphology of these glands will change in accordance with the patient's menstrual cycle.
Occasionally endometriotic glands and stroma are present immediately under the surface colonic glands. Care must be taken not to diagnosis this as invasive colonic adenocarcinoma!
This same patient showed ulceration of the surface with replacement by granulation tissue due to endometriosis. An endometriotic gland is seen in the bottom right, while colonic glands are along the bottom left of the image.
Another example from a biopsy specimen, showing normal colonic glands (left and upper) with adjacent glands which do not appear colonic in type (lower right).
Closer inspection reveals dilated glands lined by low columnar cells in a spindled stroma compatible with endometrial stroma.
The colonic glands are reactive for CDX-2, while the adjacent endometrial glands are negative.
Likewise, the endometrial glands and stroma show strong nuclear staining for estrogen receptor, confirming their origin.
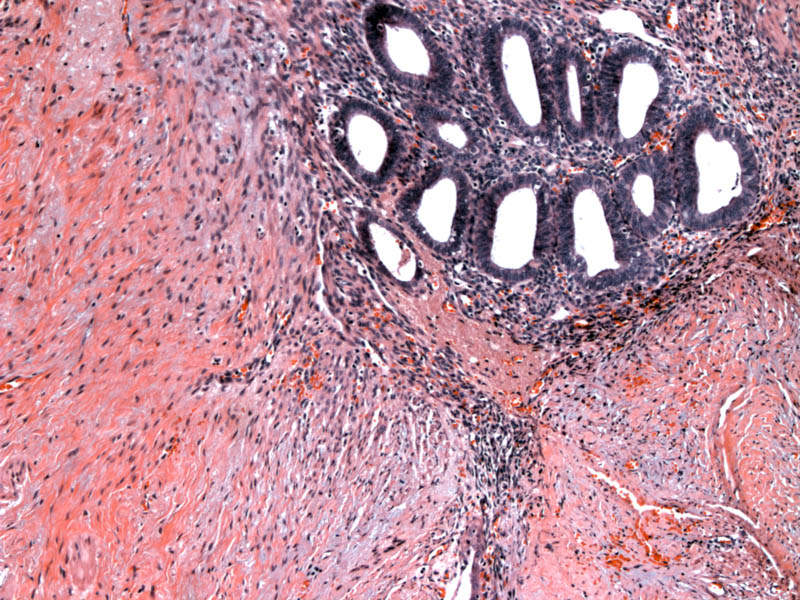
While mucosal involvement is evident on the biopsy, the subsequent segmental resection clearly shows transmural involvement of the colon by endometriosis.
Nodules of endometriotic glands studded the mucosa, interrupting the normal colonic glands. One can easily see how these glands could result in erosions and bleeding.
But as expected with endometriosis, extensive involvement of the muscularis was also seen.
The gross appearance of endometriosis may vary, depending on the location of the ectopic glands and stroma within the bowel wall.
- If the endometriosis is located on the serosa or subserosa, this may elicit serosal adhesions and serosal puckering due to subserosal fibrosis.
- If located in the muscularis propria, there can be smooth muscle hypertrophy, similar to adenomyosis seen in the uterine myometrium. On gross inspection, there may be a whorled mural thickening and can appear as a solid mass, mimicking a stromal tumor.
- If the glands are located in the submucosa or mucosa, the lesions may cause a polypoid mass simulating primary colon cancer.
Microscopically, look for ciliated columnar cells of endometrial glands without mucin and associated endometrial stroma to distinguish colonic epithelium from endometrial glandular epithelium. In cases where the endometriosis blends imperceptibly with colonic mucosa to create a picture of dysplasia, IHC panels will be helpful.
Affects reproductive age women; up to 40% of patients with pelvic endometriosis with have endometriosis in their GI tract.1 The majority of cases are asymptomatic. However, if the implants are large with significant adhesions, patients may experience abdominal pain and even bowel obstruction. Because most of the implants occur in the serosa or subserosa, rectal bleeding is less common. However, this may occur if the implants are locate in the mucosa. Therefore, the clinical presentation may be similar to diverticulitis, inflammatory bowel diseases or even primary colon cancer.
Implants tend to be located in the portions of bowel closest to the uterus, with large bowel and rectum accounting for 70% of cases.3 15% of cases affect the appendix and can mimic appendicitis, however, a good clue to consider endometriosis is that the pain is cyclic, waxing and waning with the menstrual cycle.
Pain medication and hormonal therapy. Surgery may be required for rare complications such as bowel obstruction or perforation.
Benign. There may be morbidity due to adhesions, a common complication of endometriosis and rarer complications listed above. Malignancy rarely arises from endometriosis and are most often endometrioid adenocarcinoma, clear cell carcinomas, and less likely other tumors.3
• Colon : Adenocarcinoma, Conventional Type
1 Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 251-3.
2 Odze RD, Goldblum JR, Crawford, JM. Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas. Philadelphia, PA: Elsevier; 2004:368-9.
3 Fenoglio-Preiser CM, et al. Gastrointestinal Pathology: An Atlas and Text. 3rd Ed. Philadelphia, PA: Lippincoott Williams & Wilkins; 2008: 878-881.