
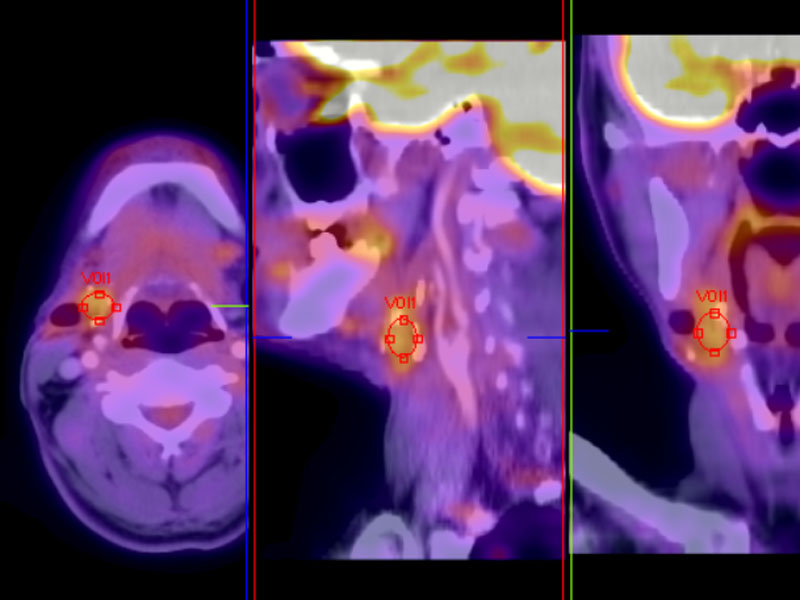
PET scan shows a nodule in the posterior submandibular gland.
Sometimes the FNA is relatively straightforward as in this instance. Spherical balls of myxoid matrix are appreciated, along with a cellular population consisting of basaloid cells with hyperchromatic nuclei and scant cytoplasm.
Other cases may yield only cohesive clusters of cells, this time with a smooth rim outlining a nest. The lack of PAS positive material around the cell nests makes the diagnosis difficult.
This histologic image better illustrates the dual cell population. Ductal cells have more abundant pink eosinophilic cytoplasm (arrow) whereas the basaloid myoepithelial cells (the majority of the cellular component) has scant to clear cytoplasm with round to angulated nuclei.
Perineural invasion is an extremely common feature. Tubules of malignant cells growing around nerves can be appreciated in this image.
The neoplasm is poorly circumbscribed, with its cribriform structures infiltrating through adjacent fat. Note again the presence of pinkish ductal cells within the cribriform island (upper right).
Another example shows less demarcated cribriform islands, but pseudocystic spaces with basophilic substance (basement membrane material elaborated by the noeplastic myoepithelial cells) are still evident in these more solid areas.
Again, another area with a slightly more solid pattern and semi-formed pseudocystic spaces is seen in this tumor.
Well-demarcated islands of cells growing in a cribriform pattern. Note the hyalinized stroma, a common feature of ACC.
This tumor produces basement membrane material which is unusually excessive, forming pink nodules.
A jumbled admixture of basaloid cells, ductal cells (upper right image -- they have eosinophilic cytoplasm) and hyalinzed stroma makes it hard to recognize as ACC. Thankfully, other areas of the tumor will have more characteristic features.
c-kit stains the ductal cells, highlighting these structures among a background of myoepithelial cells. The overexpression of c-kit in adenoid cystic carcinomas has lead to speculation that tyrosine kinase inhibitor (Gleevec) may be useful as therapy (Vila, 2009). c-kit missense point mutations have been detected in seven of eight cases in one study (Vila, 2009)
c-kit (CD 177) has been shown to be positive in adenoid cystic carcinomas (shown here), but also may stain polymorphous low grade adenocarcinomas and monomorphic adenomas (Edwards, 2003). Therefore, although some controversy still exists, it appears that c-kit interpretation should be with caution and in the correct clinical and morphological setting. Of note, one study found that c-kit staining in PLGA is seen less often and when present seem to be of lesser intensity, relative to ACC (Beltran, 2006).
p63 stains the abluminal peripheral cells strongly, the pattern of which is typical for this tumor.
Needle aspiration yields solid sheets arranged in a three dimensional structure. The sheets are composed of basaloid cells with relatively scant cytoplasm.
The corresponding tumor histology for this pap stained FNA confirms large solid areas with focal cribiform structures as suggested.
A higher power of this same tumor shows relatively uniform cells. Note that this tumor lacks the hyaline stromal component which helps define it cytologically.
The c-kit is diffusely positive in this tumor. While the tubular and cribiform types generally show c-kit in the ductal cells, in the solid variant the myoepithelial cells are modified such that they often show a diffuse staining pattern.
Adenoid cystic carcinoma (ACC) accounts for approximately 10% of malignant salivary gland neoplasms and is the most common malignant tumor of the submandibular and minor salivary glands. ACC arises from the intercalated salivary duct system and has an uncanny ability to infiltrate locally and involve nerves and bone. It is an insiduous tumor that will eventually cause the death of the patient. Three main histologic patterns are seen:1-3
(1) Cribriform/cylindromatous pattern (most characteristic): Most characteristic pattern and usually present, albeit focally. This pattern consists of smooth-contoured well-demarcated islands of basaloid cells (modified myoepithelial cells) punctuated by round pseudocystic spaces. This leads a 'Swiss cheese' look to the cribriform structures. The pseudocysts contain eosinophilic hyaline material (PAS-positive, diastase-negative) and/or basophilic mucoid material (Alcian blue-positive). These substances are elaborated by the myoepithelial cells and represent reduplicated basement membrane material.
(2) Tubular pattern: Consists of a tubules with an inner layer of ductal cells (eosinophilic) and an other layer of myoepithelial cells (clear cytoplasm, irregular angulated nuclei). The tubules are embedded in a myxohyalinized stroma.
(3) Solid variant: Consists of sheets and larger islands of closely packed basaloid cells, which may exhibit a greater degree of nuclear atypia compared to the cribriform and tubular variant. Very few pseudocystic spaces or tubular structures are seen. Central comedonecrosis is a common finding.
Note that the above patterns are usually found in combination. The cellular component largely comprises of basaloid myoepithelial cells which have round or angulated nuclei and scant or clear cytoplasm. Ductal cells, the other cellular component, line the tubules on the luminal side and contain more abundant eosinophilic cytoplasm. Mxyohyalinized stroma of the tumor surrounds the cellular portion, and occasionally, may be so abundant as to 'strangulate' the tubules and islands to created an attenuated lace-like pattern.
IHC studies reveal that the myoepithelial cells are immunoreactive for cytokeratin, S-100 (patchy staining) calponin, SMA and p63 (nuclear staining). The ductal cells can be highlighted with LMW cytokeratins (strong staining), CEA, EMA and c-kit (CD117).1,2
Peak incidence is between age 40-60 with a slight female preponderance (3F:2M). Minor salivary glands of the mouth, especially the palate and upper areodigestive tract are involved in 50% of cases. Other common locations include the parotid gland (21%), submandibular gland (13%) and the sinonasal tract (11%).1,2
The typical clinical presentation is that of a slow-growing tumor. Tenderness and pain may occur as this tumor has a strong predilection for neural invasion. In fact, facial nerve palsy may be the first presenting symptom.
Grossly, a tan, firm and fleshy mass is seen. A small tumor may appear well-circumscribed and innocuous, which often belies the true extent of tumor. In many cases, the tumor has invaded beyond what is clinically apparent.
Wide local excision is the cornerstone of treatment. Adjuvant radiation is used, but with variable results.
The progression of ACC is insiduous and relentless. Long-term prognosis and poor and eventually, the majority of patients (80-95%) die from the tumor after multiple recurrences and metastases. 5 year survival rates range from 60-75%, however, the 10 year survival rate drops to 30-54%.1
Main prognostic indicators include tumor size, stage and site. It appears that the tubular and cribriform patterns have a more favorable outcome, whereas the solid pattern suggests a more aggressive tumor, especially if encompassing over 30% of the tumor. Tumors located in the submandibular gland have a poorer prognosis compared to those in the parotid gland. Distant metastases is seen in the lung, bone, brain or liver in 60% of cases, however, local nodal metastases is much less common.1,2
• Lung : Adenoid Cystic Carcinoma
• Adnexal : Adenoid Cystic Carcinoma
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 280-284.
2 Thomspon LDR. Endocrine Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2006: 339-345.
3 Vila L, Liu H, Al-Quran SZ et al. Identification of c-kit gene mutations in primary adenoid cystic carcinoma of the salivary gland. Mod Pathol. 2009 Oct;22(10):1296-302. Epub 2009 Jul 17.
4 Edwards PC, Bhuiya T, Kelsch RD. C-kit expression in the salivary gland neoplasms adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and monomorphic adenoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 May;95(5):586-93.
Beltran D, Faquin WC, Gallagher G, August M. Selective immunohistochemical comparison of polymorphous low-grade adenocarcinoma and adenoid cystic carcinoma. J Oral Maxillofac Surg. 2006 Mar;64(3):415-23.
Slides courtesy of Dr. Lida Crooks, VAMC Albuquerque, NM.