
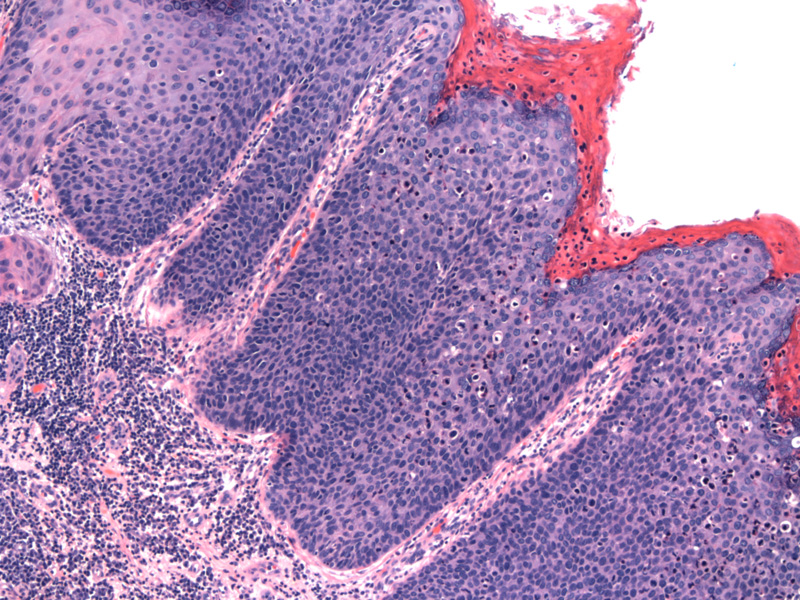
High grade lesion of the vulva (VIN, classic type) is shown here. There is acanthosis with overlying parakeratosis. Full thickness atypia with loss of maturation is evident. The crowded dysplastic squamous cells have high N/C ratio, scant cytoplasm, hyperchromatic and pleomorphic nuclei.
Not infrequently, HGVIN extends into underlying adnexal structures, which in some instances may be confused with invasion. In this image, the surface is along the top, and complex VIN invades a sebaceous gland, creating a downward growth of dysplasia, which is not invasive.
Vulvar intraepithelial neoplasia (VIN) is the precursor lesion to invasive squamous cell carcinoma, the most common malignancy in the vulva. Older terms include Bowen's disease, squamous dysplasia and squamous cell carcinoma in situ.
There are two distinct pathways in the pathogenesis of VIN: (1) the HPV-related pathway, which leads to 'classic' VIN and (2) the non-HPV related pathway, so called the 'differentiated' or 'simplex' type of VIN.
VIN, classic type: This variant is associated with high-risk HPV subtypes (namely 16, 18 and 33). 30% of women have co-existing HPV-related squamous lesions in the cervix or vagina. Superficially invasive squamous cell carcinoma is identified in 20% of VIN cases upon careful histologic examination.1
The classification of VIN classic type is currently evolving. Historically, VIN I to III (corresponding to cervical neoplasia) was used to stratify these lesions. However, the ISSVD Vulvar Oncology Subcommittee has proposed that (1) VIN be used to define high-grade VIN lesions which combines VIN II and VIN III, and (2) the term VIN I should be dropped altogether. Sorting out low-grade VIN lesions has been problematic. Previously VIN I was defined as atypia confined to the lower layers of the epithelium, however, these changes are also seen in the differentiated variant of VIN as well as inflammatory conditions. Therefore, low-grade VIN lesions should be described as 'flat condyloma acuminatum' if viropathic changes are present. Needless to say, the definition of low-grade VIN (previously VIN I) is still very murky and confusing.1,2
Variants of the classic 'bowenoid' VIN include warty (condylomatous) and basaloid types. The warty type consists of 'spiky' projections of hyperplastic epithelium with prominent koilocytic change. The basaloid type consists of a proliferation of small dark squamous cells (parabasal-type); koilocytia atypia is uncommon in this variant.2
VIN, simplex type: Occurs in older women when compared to the classic type. It is presumably not associated with HPV infection and frequently occurs in the context of lichen sclerosus.
Microscopically, the atypia is confined to the lower third of the epithelium, but is considered high-grade VIN due to its associated risk of progressing into invasive squamous cell carcinoma. The atypical features can be quite subtle and consist of mature-appearing kertinocytes. However, the keratinocytes on close inspection will be abnormal with abundant brightly eosinophilic cytoplasm and oddly prominent intercellular bridges. Keratin pearls and whorling of keratinocytes may be seen in the rete ridges. The nuclei are enlarged with prominent nucleoli. The basal layer will more 'typical' atypical features, consisting of hyperchromatic, crowded cells with high N/C ratios.1,2
p16 (surrogate marker for high-risk HPV) will stain positively in classic VIN. p53 staining is confined to the basal epithelium in normal squamous mucosa and lichen sclerosus. However, in differentiated VIN, there will be suprabasilar extension of p53 positive nuclei. Molecular studies have failed to detect HPV in well-differentiated VIN.2,3
Classic type: Age of diagnosis has been decreasing in the last few decades and currently, the mean age at diagnosis is 40. Risk factors are the same as for HPV-related lesions in the cervix and vagina and include early age of first sexual encounter, multiple partners, smoking, immunosuppression and HIV infection.
Differentiated (simplex) type: occurs at a later age (6th and 7th decades). Accounts for 10% of VIN and associated with inflammatory conditions such as lichen sclerosis.2
Both types may be asymptomatic or present with itching, burning and soreness. The clinical appearance varies from flat to verrucous lesions, which may be erythematous, pigmented and/or ulcerated.
While wide local excision is the classic treatment modality, this approach can be disfiguring and result in dyspareunia. In addition, high recurrence rates and multifocal lesions make wide local excision less preferred. Laser ablation and cryotherapy are alternative treatment modalities.
In classic VIN, the average interval from diagnosis of high grade dysplasia to invasive squamous cell carcinoma is approximately 4 years.2 There is a high-risk of local recurrence after excision, making follow-up care an important part in the management of this condition.
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 752-3.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 44-52.
3 Yang B, Hart WR. Vulvar intraepithelial neoplasia of the simplex (differentiated) type: a clinicopathologic study including analysis of HPV and p53 expression. Am J Surg Pathol 2000 Mar;24(3):429-41.