
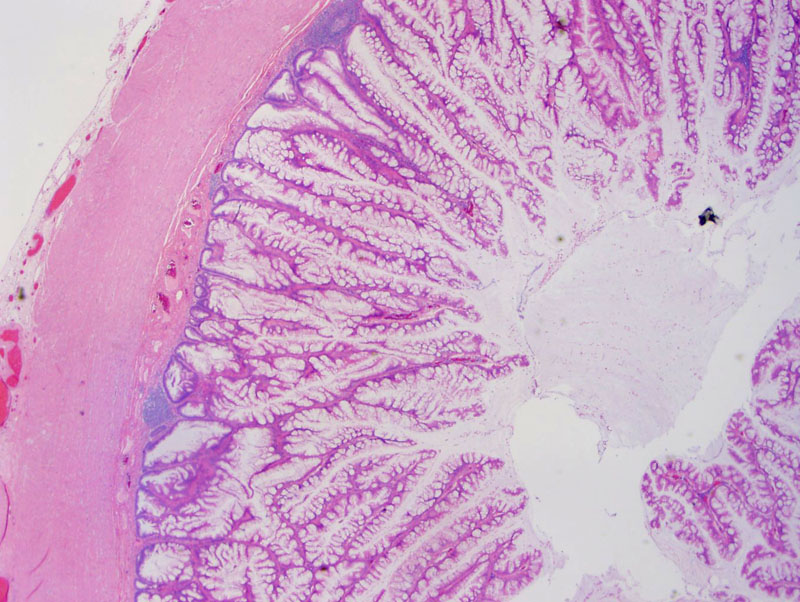
Low-grade mucinous columnar epithelium lines the appendix. Note the abundant mucin produced by this tumor. The mucin is still confined to the appendix, although it may appear otherwise to the a tangential cut of this section and dissection of mucin into the appendiceal wall.
Undulating columnar epithelium is seen, but there are no complex papillary or cribriforming structures. There is abundant luminal extracellular mucin.
The cytology is of the glandular epithelium is pseudostratified, hyperchromatic but still polarized. Note that this lining is adenomatous, which separates this mucinous adenomas from hyperplastic lesions (which do NOT exhibit any dysplasia). It is important to note, however, that mucinous neoplasms low-grade cytology may demonstrate invasion elsewhere and thus is actually a mucinous adenocarcinoma. Although mucinous adenocarcinomas often demonstrates high-grade cytology, the tumor is often heterogeneous with foci of low-grade epithelium. Thorough sampling or entire submission of the appendix is key to identifying invasion.
This other case harbors acelluar mucin dissecting into the appendiceal wall. This is often mistaken for invasion. However, true invasion demonstrates infiltrative and jagged glands, whereas dissecting or herniating mucin and epithelium has a broad pushing border. Note the dystrophic calcification Image
The classification of mucinous tumors of the appendix is still in flux, however, the scheme proposed by Pai and colleagues focuses on a few key features (cytologic atypia, presence of cellular or acellular extra-appendiceal mucin and invasion) appears to have clear prognostic implications and stratifies the various subgroups into different survival rates.
The classification of appendiceal mucinous neoplasms has been problematic for several reasons. Cytologically low-grade mucinous neoplasms within the appendix appear to behave benignly, however, once mucin +/- adenomatous epithelium escapes from the confines of the appendix, morbidity and mortality increases significantly even if the cytology remains low-grade. Evaluation of lesions is complicated by the fact that viscid mucin can dissect through the appendiceal wall, creating diverticuli and herniations of the epithelium that often mimic invasion. Furthermore, when processing the specimen, the sticky mucin can adhere to tissues and appear on the glass slide as extra-appendiceal mucin.
Pai and colleagues (2009) studied 116 cases of appendiceal mucinous neoplasms and derived a concise set of histologic features with important prognostic implications.1 In summary, Pai divided mucinous neoplasms into four groups using the following features: cytologic atypia of glandular epithelium, presence of extra-appendiceal cellular or acellular mucin (celluar mucin contains adenomatous epithelium whereas acellular mucin does not) and invasion (defined and infiltrative, jagged adenomatous epithelium beyond the muscularis mucosa of the appendix).
The authors were careful to stress that extra-appendiceal mucin must elicit a response from surrounding tissues in the form of granulation-like tissue and neovascularization. One must careful of overcalling mucin and adenomatous epithelium that herniate and dissect through the appendiceal wall as invasion. To unequivocally diagnose invasion, jagged infiltrative glands beyond the muscularis mucosa must be identified.
As noted in the chart above, mucinous neoplasms splits out into four groups:
- Mucinous (cyst)adenoma: Low-grade mucinous neoplasms confined to the appendix
- Low-grade mucinous neoplasms with low risk of recurrence (LG-LR): Features identical to mucinous adenomas, with the added component of acellular extra-appendiceal mucin
- Low-grade mucinous neoplasms with high risk of recurrence (LG-HR): Same as LG-LR, but the extra-appendiceal mucin contains neoplastic epithelium.
- Mucinous adenocarcinoma: Presence of invasion; usually, but not always, exhibits high grade cytology and complex architecture.
Note that mucinous adenomas and mucinous cystadenomas most likely represent the same entity, as the neoplastic epithelium in a noncystic adenoma eventually generates enough mucin to cause luminal dilatation and thus, become a cystadenoma.2
Pseudomyxoma peritonei is often associated with mucinous neoplasms of the appendix. Some authors define it as any mucin extravasation into the peritoneal cavity. Others require the presence of malignant epithelium within the mucin that adhere to peritoneal surfaces and proliferate. In either instance, it appears that presence of diffuse mucin in the peritoneal cavity (versus a localized collection of mucin) predicts a more aggressive tumor.
Ovarian mucinous tumors may also cause pseudomyxoma peritonei, however, in most instances where both ovarian and appendiceal mucinous neoplasms are found in association pseudomyxoma peritonei, it is usually attributed to a primary appendiceal neoplasm.3
In terms of overall survival, patients with mucinous adenomas and LG-LR were all alive at 1 year, 3 year, 5 year, and 10 year followups. Patients with LG-HR, however, had a 1 year, 3 year, 5 year, 10 year survival rates of 96%, 91%, 79% and 46% respectively. Patients with mucinous adenocarcinomas had 1 year, 3 year, 5 year, 10 year survival rates of 85%, 57%, 28% and ~0% (either lost to followup or deceased), respectively.1
Thus, on a Kaplan-Meier curve, the criteria which Pai and colleagues used to stratify the four subgroups correlates well with both disease free survival (data not discussed here) and overall survival. Mucinous adenomas and LG-LR do very well; LG-HR have higher rates of disease recurrence and increase mortality; mucinous adenocarcinomas have a dismal outcome.
Of note, mucin deposits with or without neoplastic epithelium located beyond the right lower quadrant is associated with a worse prognosis.
1 Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal Mucinous Neoplasms: Clinicopathologic Study of 116 Cases with Analysis of Factors Predicting Recurrence. Am J Surg Pathol 2009; Epub ahead of print.
2 Riddell RH, Petra RE, WIlliasm GT, Sobin LH. Tumors of the Intestines: Atlas of Tumor Pathology.Third Series, Fascicle 32. Washington DC; AFIP: 2002; 241-248.
3 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 871-2, 1097.