
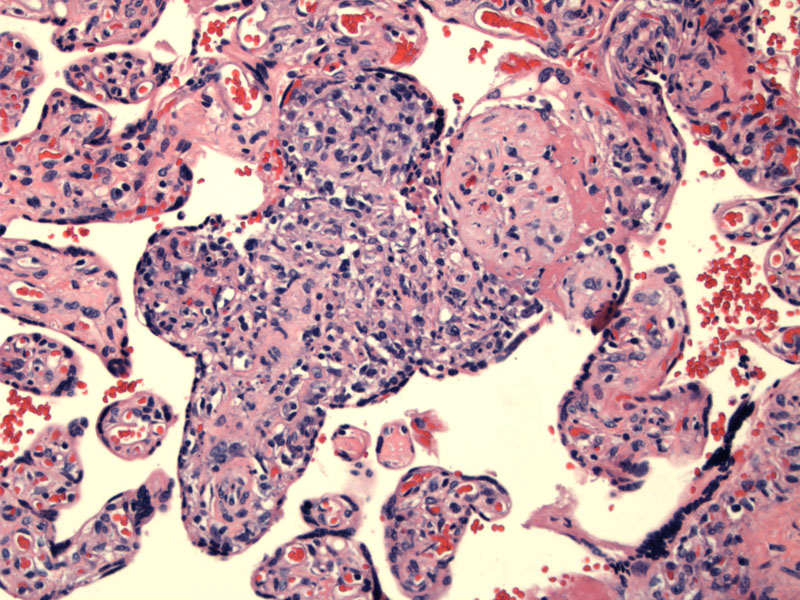
Infiltration of villi by mononuclear cells can be seen. Infectious villitis (syphilis or CMV) would have a lymphoplasmacytic infiltrate, whereas VUE (villitis of unknown etiology) has a histiocytic predominance.
Villi are hypercellular due to endothelial and fibroblastic proliferation. In infectious villitis, the villi may be somewhat bulky and enlarged. A vigorous inflammatory infiltrate can be seen; note the absence (obliteration) of vessels in the villi.1
Again note the increase in lymphoid cells within the villi and difficulty in locating capillaries in much of the villous surface area (1-2 o'clock).
Chronic villitis, defined as a chronic inflammatory infiltrate in the villi, are divided into two main categories.
(1)Infectious villitis: Maternal infections are transmitted either hematogenously or transplacentally. Organisms include TORCH organisms (Toxoplasmosis, Rubella virus, CMV and Herpes Simplex virus) as well as spirochetes, parasites and other viruses. 90% of infectious villitis are due to CMV and syphilis.1
In syphilis infection, the spirochete Treponema pallidum can be visualized by immunoflorescence. Interestingly, the placenta is increased in weight. Microscopically, the villi are enlarged due to endothelial and fibroblastic proliferation. The villi appear hypercellular with a mononuclear infiltrate with prominent plasma cells. In CMV infection, there is also a lymphoplasmacytic infiltrate of the villi. A careful search may reveal nuclear and cytoplasmic CMV inclusions in enlarged cells. Infected cells include capillary endothelial cells, villous stromal cells, amnion and decidual cells. Hemosiderin deposits in the stroma is also highly characteristic.1
(2) Villitis of unknown etiology (VUE): Chronic villitis is a common finding, occurring in up to 10% of all placentas. A subset can be attributed to the aforementioned infectious organisms, however, the majority of cases do not have a specific etiology and are thus designated villitis of unknown etiology.
Two theories of pathogenesis have been proposed. The first theory suggests that VUE is actually an infectious disease, however, the agent is unrecognized and non-detectable by the usual methods of placental examination. The histologic overlap between certain viral infections of the placenta and VUE support this theory.
The second (favored) theory posits that VUE is an immune process, akin to graft versus host disease whereby the placenta is the 'graft' being attacked by the maternal immune system. Features that support this 'rejection' theory include: (1) concentration of inflammatory activity at the maternal-fetal interface (basal villi in the maternal floor of the placenta); (2) a significant percentage of infiltrating lymphocytes are maternal T-cells from the intervillous space that gain inappropriate access to the villi; (3) a predominance of histiocytes (versus a plasma cell infiltrate in infectious villitis; (4) familial association; (5) association with autoimmune disease in the mother.1
Due to diffuse and multifocal involvement of the placenta, VUE can compromise nutrient transfer, thus, leading to growth restriction in up to 1/3 of cases. Depending on the infectious organism associated various congenital syndromes may result.
1 Baergen RN. Manual of Benirschke and Kaufmann's Plathology of the Human Placenta. New York, NY: Springer; 2005: 297-301, 308-11.
2 Redline RW. Villitis of unknown etiology: noninfectious chronic villitis in the placenta. Hum Pathol. 2007 Oct;38(10):1439-46.
