
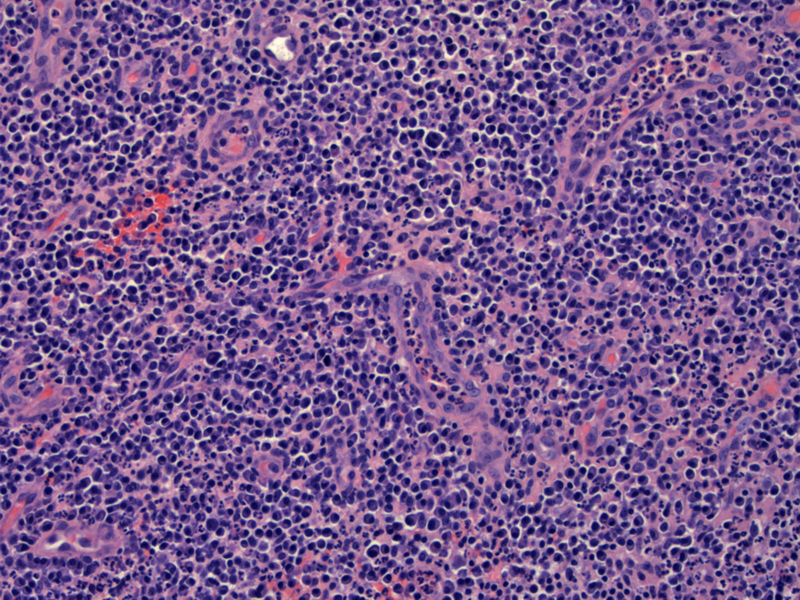
A hypervascular stroma is largely replaced by dense acute and chronic inflammatory process.
Hemorrhage and a brisk mixed inflammatory infiltrate with many neutrophils surround the vessels. The stroma is edematous.
Much of the biopsy showed large aggregates of neutrophils, admixed with blood.
A mixed inflammatory infiltrate is seen in both acute and chronic endometritis. In simplistic terms, plasma cells predominate in chronic endometritis and neutrophils predominate in acute endometritis. Thus, the diagnosis of acute endometritis requires a dense infiltrate of inflammatory cells with a prominent neutrophils. Infiltration and destruction of glandular epithelium is seen and microabscesses (collections of neutrophils) are focally present. Acute endometritis most often occurs as a complication following uterine instrumentation or childbirth. Endometritis as part of pelvic inflammatory disease is often preceded by a gonococcal or chlamydial infection (Sternberg).
Pyometra (pyometrium) is defined as pus in the uterine cavity due to obstructed drainage. The cause of obstruction is most often a uterine malignancy, thus, pyometra is generally seen in postmenopausal women. It can be seen in younger women as a result of congenital genital tract anomalies or cervical stenosis. Occasionally, benign conditions such as a large leiomyoma can cause obstruction. Pyometra presents with postmenopausal bleeding, purulent vaginal discharge and lower abdominal pain. Some patients are asymptomatic. Rarely, pyometra may be a cause uterine rupture and an acute abdomen (Yildizhan, Muram).
Patients with endometritis typically present with high fevers, abdominal pain, bloody foul smelling vaginal discharge, a tender uterus. These patients often have a recent history of uterine instrumentation or childbirth. If the patient is remote from instrumentation or childbirth, consideration should be given towards a case of pelvic inflammatory disease rooted in gonorrhea or chlamydia.
Endometritis is typically treated with a two week course of broad spectrum antibiotics. If the endometritis is part of pelvic inflammatory disease, care is taken ensure adequate treatment of any preceding gonorrhea or chlamydia. If the patient is recently postpartum and presents with endometritis, consideration should be given towards possible retained products of conception that can serve as a nidus for the infection. Infections not responding to antibiotic therapy may require hysterectomy.
Endometritis is most often successfully treated so long as treatment is prompt. If the infection is left unchecked it may result in sepsis and death. Chronic sequelae of endometritis rarely may include asherman's syndrome. Chronic sequelae of pelvic inflammatory disease may include pelvic adhesions, chronic pelvic pain, and infertility.
→In acute endometritis, there is a infiltration of neutrophils. In chronic endometritis, plasma cells predominate.
→Often, there is a history of instrumentation or childbirth in acute endometritis. Pelvic inflammatory disease may also involve the endometrium.
Muram D, Drouin P, Thompson FE et al. Pyometra. Can Med Assoc J 1981 September 15; 125(6): 589–592.
Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2450.
Yildizhan B, Uyar E, Sişmanoğlu A, et al. Spontaneous perforation of pyometra. Infect Dis Obstet Gynecol 2006.