
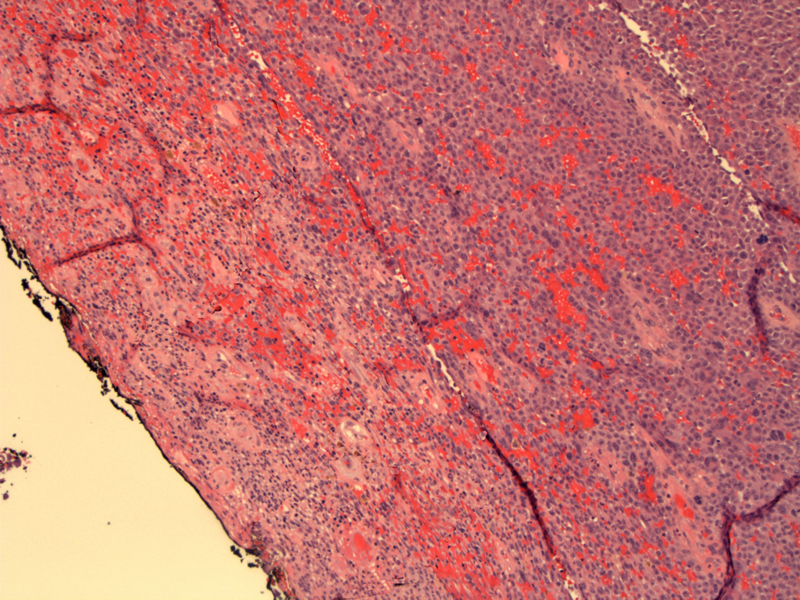
Eroded surface epithelium no longer present (inked on the left). An undermining melanocytic proliferation is seen (right image).
A diffuse sheet of spindled melanocytes is seen the dermis, with areas of heavy pigmentation.
The spindled melanocytes with fusiform vesicular nuclei are only mildly atypical, a pattern typical of acral-lentiginous melanoma.
Melanoma is the second most common malignant neoplasm in the vulva (squamous cell carcinoma is the most common). Risk factors for vulvar melanoma are poorly understood; sun exposure, parity and genetics do not appear to play significant roles in oncogenesis. Up to 35% of vulvar melanomas are amelanotic.1
Microscopically, most vulvar melanomas fall into one of three histologic patterns: acral lentiginous, superficial spreading, nodular and rarely, desmoplastic. Acral lentingous appears to the most common pattern, although some reports differ on this point.2 Briefly, acral lentingous consist of an intraepidermal component (large epithelioid atypical melanocytes in nests with pagetoid spread) and an dermal component (spindle-shaped cells that may only be mildly atypica); nodular type lacks a radial growth phase; superficial spreading consists of atypical epitheliod melanocytes scattered widely throughout the epidermis and also involving four or more contiguous rete ridges.
Remember that Clark staging was developed for cutaneous skin and the mucocutaneous skin of the vulvovaginal region lacks a papillary dermis and reticular dermis. In terms of reporting, Clark staging can be used for hairbearing skin of the vulva, and a modified scheme developed by Chung can be used. Breslow thickness is measured from the base of the granular layer to the deepest point of invasion.3
The melanocytes would stain positively with S-100, HMB-45 and Melan A.
Affects older women (6th and 7th decades) when compared to melanoma in sun-exposed areas. Most arise in the clitoris (31%) followed by labia majora (27%) and labia minora.1
As with cutaneous melanoma, prognosis depends on depth. However, vulvar melanomas tend to have a poorer prognosis with compared to extragenital melanoma. Overall median survival is 41 months. 5-year survival ranges from 47% to 54%.2
1 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 71-5.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 739.
3 Kurman RJ, Norris HJ, Wilkinson E. Tumors of the Cervix, Vagina and Vulva: Atlas of Tumor Pathology. Third Series Fascicle 4. Washington DC; AFIP: 1990: Section 7.5.2.