
Case 1 - The tumor consists of an epithelial neoplasm showing overt cytologic features of malignancy, without defining features of a thymoma. They are similar to carcinomas from other organs, and thus, must be distinguished from them.
While this tumor appears fairly well-differentiated, the morphologic spectrum of these tumors ranges from this appearance through those that are high-grade, poorly differentiated malignancies.
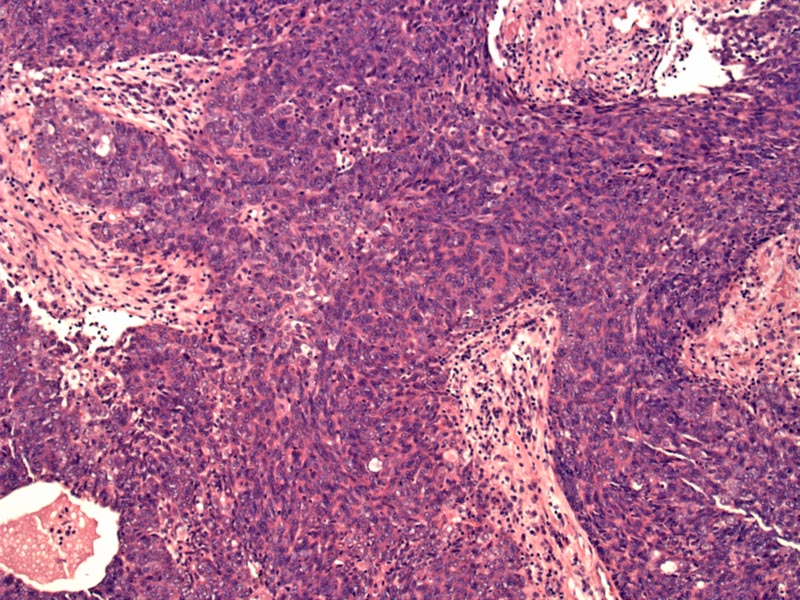
Case 2 - Here's another case. The neoplastic epithelial cells are somewhat squamous in appearance, which is the most common histologic subtype. The infiltrate elicits a desmoplastic stromal response.
Sclerosis is quite prominent. These thick sclerotic bands are perhaps reminiscent of the fibrous septae separating lobules in type B thymomas, however, the epithelial component is fairly nonspecific and lymphocytes are sparse to absent.
Comedonecrosis can be seen within the epithelial islands.
Thymic carcinomas (previously designated type C thymoma) do not exhibit any of the characteristic features defined for type A and type B thymomas. Features such as abortive Hassall corpuscles, pseudorosettes and glandular spaces are uncommon. Furthermore, unlike thymomas in which paraneoplastic syndromes such as myasthenia gravis occur in 1/3 of cases, this association is rare in thymic carcinomas (Rosai, Suster).
Not only is the morphology poorly defined, but thymic carcinomas exhibit a variety of histologic subtypes that may mimic carcinomas from other organs. Thus, assigning this diagnosis requires a thorough clinical evaluation to rule out the possibility of a thymoma as well as a primary malignancy elsewhere (Suster).
IHC markers will be helpful, especially CD5, CD117 and CD70. These markers are more likely to be positive in thymic carcinomas and negative in thymomas (Fletcher, Rosai). Interestingly, unlike GIST, overexpression of KIT does not necessarily indicate gene mutation in thymic carcinoma (Yoh). TTF-1 will be helpful in distinguishing between lung tumors as both may be located in the anterior mediastinum (Fletcher).
Thymic carcinoma occurs in all age groups but peak incidence is between 30 and 60 years of age with a slight male predominance (M:F ratio of 1.5:1)(Fletcher, Suster). Patients experience symptoms attributable to the anterior mediastinal mass such as chest pain, shortness of breath, and superior vena cava syndrome. Other symptoms are nonspecific and include weight loss, fatigue, fever and anoxeria. Exceptionally, there may be an association with myasthenia gravis (Suster).
Multimodality therapy is often employed for treatment of thymic carcinomas, which frequently are not radically resectable at diagnosis (Rajan).
Thymic carcinomas differ from thymomas in that they follow an aggressive clinical course. Metastatic disease may be present at the time of initial diagnosis, with involvement of bones, lung, liver, pleura, and lymph nodes. Note that the histologic subtype carries prognostic significance. Complete resection is a highly important prognostic factor for survival. The addition of neoadjuvant chemotherapy with or without radiation improves the rates of complete surgical resection.
Rajan A, Giaccone G. Treatment of advanced thymoma and thymic carcinoma. Curr Treat Options Oncol. 2008 Dec;9(4-6):277-87.
Moran CA, Suster S. Thymic carcinoma: current concepts and histologic features. Hematol Oncol Clin North Am. 2008 Jun;22(3):393-407.
Suster S., Rosai J.: Thymic carcinoma. A clinicopathological study of 60 cases. Cancer 67. 1025-1032.1991
Yoh K, Nishiwaki Y, Ishii G, Goto K, Kubota K, Ohmatsu H, Niho S, Nagai K, Saijo N. Mutational status of EGFR and KIT in thymoma and thymic carcinoma. Lung Cancer. 2008 Dec;62(3):316-20.