
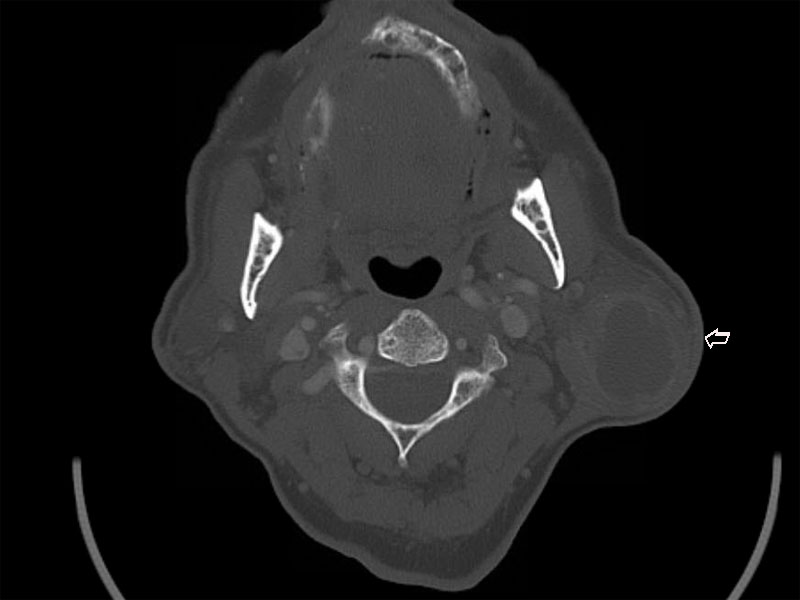
CT scan reveals a 3cm hypodense mass is seen in the tail of the left parotid gland (arrow).
A myxoid appearing oval neoplasm is appreciated. The section on the right implies a cystic component, with a more fleshy appearance, the latter compatible with the tumors lymphoid component.
A Diff-Quik stain demonstrates a cluster of Hurthle cells with their abundant cytoplasm. There is mild variation in nuclear size and shape; the nuclei are about twice the size of a RBC.
An FNA reveals a watery background with debris, consistent with the fluid in the cystic areas. The orangophilic single cell at 1-2 o'clock may represent a rare squamous metaplastic cell, which may be present in Warthin tumor.
Another area of the background shows macrophages, lymphoid cells and granular proteinaceous debris.
Flat sheets of polyhedral Hurthle (oncocytic) cells in a honeycomb pattern is the distinctive finding in a Warthin tumor in an FNA. The cytoplasm can stain green, reddish-brown (seen here) or even blue with the Papanicolaou method. Occasionally a prominent nucleolus may be appreciated.
Image contains a diagnostic combination of Hurthle cells (oncocytic columnar cells) arranged in a honeycomb sheet on left and lymphoid background.
Here is the classic morphology on the cell block. Pink tall columnar cells oriented toward the cystic lumen with a layer of basal cells -- this strip of pink epithelium overlies a dense lymphoid infiltrate.
A double layer of oncocytic epithelium lines papillary and cystic structures.
The dense lymphoid stroma often looks similar to a normal lymph node complete with lymphoid follicles and germinal centers -- this tissue may even function like a regular lymph node.
The intensity of the lymphoid stroma can be quite dense, as seen in this polypoid extrusion of lymphoid material with a large reactive germinal center. In contrast, the adjacent attenuated epithelium is largely devoid of underlying lymphoid cells.
The stroma can vary as well, and in this field it shows more dense sclerosis.
The sclerotic stroma can become inflamed, showing not just the expected lymphocytes but the addition of plasma cells.
Occasionally eosinophilis may also be admixed as a part of the inflammation.
In some areas, the typical bilayered oncocytic epithelium (seen at the right)lining may become attenuated, as seen to the left.
Here is the corresponding histology of the granular eosinophilic material evident on FNA. The cystic space contains proteinaceous fluid with degenerating cells, which are largely inflammatory in type.
Warthin tumor, also known as the more descriptive term papillary cystadenoma lymphomatosum, is the second most common salivary gland tumor (after pleomorphic adenoma). It has a very distinctive and unmistakable histology composed of two main components: (1) double-layer of oncocytic epithelium arranged in papillae or forming cystic structures and (2) a rich lymphoid stroma.
Warthin tumor is almost exclusively located in the parotid glands or in the periparotid lymph nodes. Grossly, the tumor is well-circumscribed with a cut surface that contains numerous small cystic spaces oozing a brownish liquid.
Microscopically, a double-layer of oncocytic epithelium (a columnar layer that is polarized toward the cystic lumens and a basal layer that separates the epithelium from the lymphoid stroma) is arranged in papillae and also lines variably sized cystic structures. Note that the papillae may be compressed into long trabecular cords, however, the features of Warthin tumor should still be very obvious. The cystic lumens may contain eosinophilic proteinaceous material and debris. Germinal centers are commonly found in the dense lymphoid stroma.1
Often occurs in the 6th and 7th decade with a definite male predominance (M:F ranging from 5-26:1). Recent epidemiologic data reveals there has been a decline of incidence in males and an increase in females, likely attributed to the trends in smoking (a risk factor for Warthin tumor).1,2
Compared to pleomorphic adenomas and monomorphic adenomas (benign tumors of the salivary gland which are usually asymptomatic), Warthin tumor is more likely to be symptomatic. Patients can present with facial weakness, pain and ear symptoms such as tinnitus and deafness. Furthermore, Warthin tumor is more likely to be multifocal (up to 20% of patients), bilateral (up to 14% of patients) and found in conjunction with other salivary gland tumors such as pleomorphic adenoma.
Excision is curative in most cases.
Recurrence rate have been reported from 4% to 25% -- this has been attributed to incomplete excision or the tumor's propensity to be multicentric. Malignant transformation to squamous cell carcinoma or low-grade B cell lymphoma occurs in 1% of patients.2
• Salivary Gland : MALT Lymphoma
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 266-269.
2 Thomspon LDR. Endocrine Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2006: 309-312.