
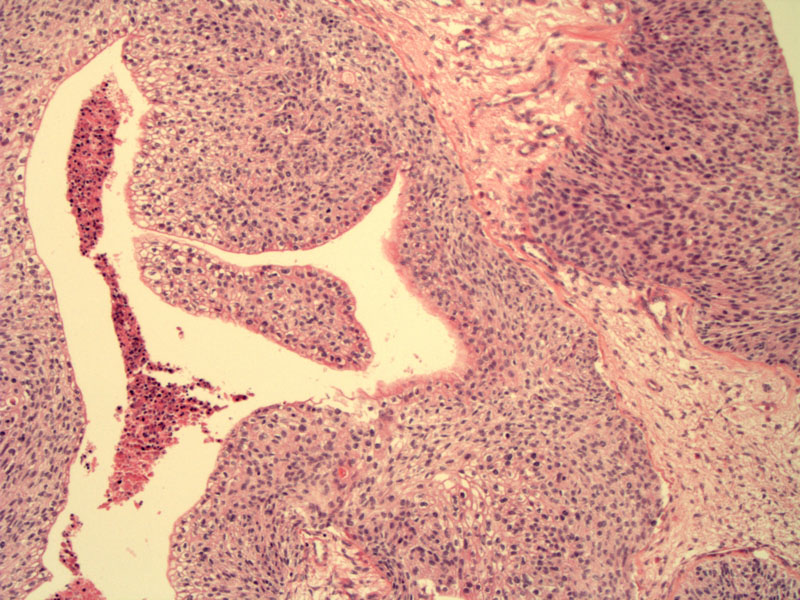
Papillary proliferations of transitional-cell type epithelium projecting into cystic lumens are typical of borderline Brenner tumor. In this image, the projections are not especially papillary, but more broad and coarse.
Atypical transitional cells, exhibiting mild to moderate cytologic atypia and loss of polarity, line the cystic lumens. Note the central necrosis. These features are consistent with a moderate to high grade borderline Brenner tumor.
The lining resembles transitional cell carcinoma and contains mitotic figures.
This different case was designated as 'proliferating Brenner tumor', which some authors call low-grade borderline Brenner tumor. There is an exuberant proliferation of transitional-type cells without nuclear atypia. In contrast, the above case of higher grade borderline tumor exhibits more prominent nuclear atypia as well as high mitotic activity and areas of necrosis.
A closer look reveals bland transitional-type cells growing in nests. Fibrous ovarian stroma can be seen on the right.
Borderline brenner tumors have also been called 'proliferating Brenner tumor'. Some authors propose that these tumors be subclassified into 'proliferative' or 'low malignant potential' based on the amount of cytologic atypia. Proliferating Brenner is basically a proliferation of bland transitional-type cells with no cytologic atypia while Brenner tumor of low malignant potential exhibit mild to moderate cytologic atypia. In his textbook, Fletcher prefers to employ the term borderline Brenner tumors to encompass both entities and add the qualifier 'low-grade' for proliferative-type tumors and 'high-grade' for tumors with more atypical features. If cytologic atypia and mitotic activity are pronounced and there is no stromal invasion, a diagnosis of intraepithelial carcinoma may be warranted.1
Up to 1/3 of Brenner tumors contain mucinous elements (mucinous glands, cysts or co-existing mucinous adenocarcinomas). Some Brenner tumors may arise from the wall of a mucinous cystadenoma. Occasionally, Brenner tumors may be associated with a dermoid cyst. Grossly, borderline Brenner tumors are cystic and unilocular or multilocular. Papillary protrusions resembling cauliflower florets protrude into the cystic lumen.2
Microscopically, broad papillary proliferations protrude into cystic lumens. The fibrovascular cores are covered by stratified transitional-type epithelium that resemble low-grade transitional cell carcinoma of the urinary tract. Mitotic figures (rare to absent in benign Brenner tumor) are present in borderline tumors. More pronounced nuclear atypia distinguishes low-grade from high-grade borderline tumors. Foci of benign Brenner tumor can be found adjacent to the borderline tumor.
Benign Brenner tumors have a peak incidence in the late 40s and early 50s. Borderline and malignant Brenner tumors occur in women who are approximately 10 years older. Borderline Brenner tumor is usually unilateral and range from 8 to 30 cm in diameter (larger than the benign counterpart).1
• Ovary : Transitional Cell Carcinoma
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 586.
2 Mills SE, ed. Sternberg's Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2569-70.