
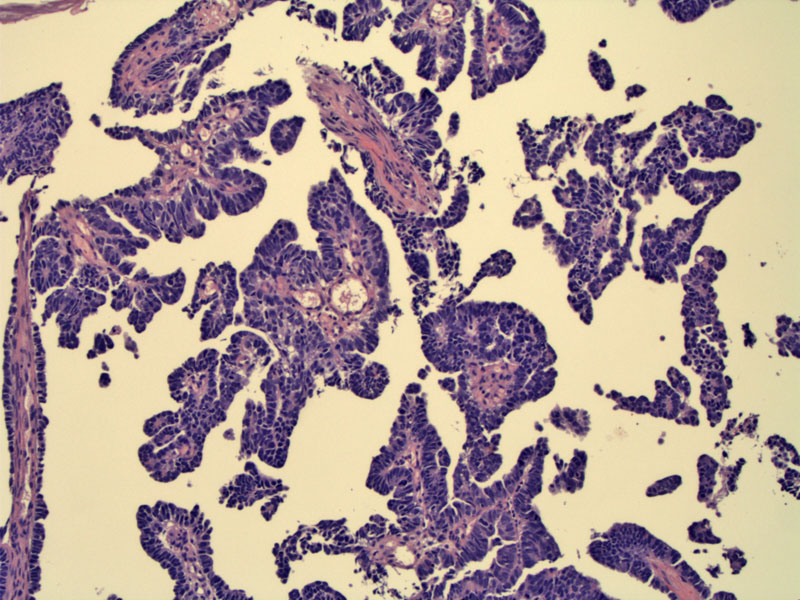
A biopsy of demonstrates the papillary architecture of this neoplasm.
The same biopsy shows diffuse nuclear p53 staining, which supports the diagnosis of a serous carcinoma.
Complex papillary structures are lined by malignant stratified cells. Invasion is present -- look within the papillary cores.
There is widespread invasion into the myometrium. A proliferation of malignant glands creating cleft-like spaces is seen.
Tubulopapillary elongated structures are lined by markedly atypical cells. Note the pleomorphism and prominent nucleoli.
Single cells or clusters of cells become detached from micropapillary tufts and are seen floating between papillae.
This image demonstrates the invasive front. Malignant glands and even single cells are dissecting freely into myometrium, eliciting a prominent desmoplastic response.
Tumor implants (on the left) are seen on the ovary.
Peritoneal washings contain numerous malignant cells.
Higher power reveals pleomorphic cells with abundant clear cytoplasm and prominent nucleoli.
Subsequently, a pleural effusion developed which showed clusters of the same malignant cells.
Serous carcinoma is often papillary in architecture, hence, the term 'papillary serous endometrial carcionma'. These tumors are highly aggressive tumor with an propensity for early peritoneal spread and deep myometrial invasion.
Serous carcinoma is the prototypical "type II endometrial carcinoma" -- these tumors are unrelated to estrogen exposure, occur in postmenopausal women, exhibit p53 alterations and carry a poor prognosis. In contrast, "type I endometrial carcinomas" (of which endometriod adenocarcinoma is the prototype) occurs in younger women (pre- and peri-menopausal), are related to unopposed estrogen exposure, exhibit PTEN and k-RAS mutations, and usually have a better prognosis than type II endometrial carcinomas.1
Microscopically, there is often a complex papillary pattern consisting of broad or slender papillae lined by cells with highly malignant cytologic features (marked pleomorphism, high N/C ratio, hyperchromasia and prominent nucleoli). Mitotic figures, giant tumor cells and psammoma bodies are frequent findings. Unlike endometrioid adenocarcinomas which are graded FIGO 1-3 depending on the amount of solid growth, serous carcinomas are not graded as they are all high grade and aggressive tumors.
Another highly distinctive feature is the propensity for the malignant glandular cells to stratify and form tufts. Single cells or collection of cells often detach from the tufts and float freely between the papillae. Although papillary formation is the most frequent architectural pattern, solid sheets of tumor cells, formation of irregular slit-spaces and glandular formations are also common arrangements.2,3
Serous carcinoma is often associated with deep myometrial invasion, however, even when absent, there is still a significant chance that the tumor has spread beyond the uterus. In fact, tumor stage and myometrial invasion has little predictive value when it comes to positive peritoneal washings. Lymphovascular invasion can be extremely subtle as well and requires a thorough and diligent search for tumor clusters within vascular spaces of the serosa, myometrium, ovaries and cervix.
Patients often present with postmenopausal bleeding, but may also present with abnormal cervical cytology, ascites, or a pelvic mass.
Uterine cancers are surgically staged with total hysterectomy, bilateral salpingo-oophorectomy, washings, and pelvic and peri-aortic lymphadenectomy. A careful evaluation of the peritoneum is especially important in papillary serous endometrial adenocarcinoma cases as rates of extrauterine spread are very high even in the presence of disease confined to the endometrium. While radiation therapy has not been shown to be of much benefit, platinum-containing chemotherapy regimens are showing promise.
This tumor is characterized by an aggressive nature and shorter overall survival compared with uterine cancer of endometrioid histology. Local and distant recurrences occur frequently, with extra-pelvic relapses most common. In a study of 129 patients of various stage, 5-year overall survival among all patients was 45.9%. Note that even among patients with no uterine invasion, staging revealed that over one third actually had stage III or IV disease (Slomovitz).
Another study reported a 5 and 10 year survival rates of 27% and 14%, respectively. This study also found that a mixed endometrioid and serous adenocarcinoma has the same poor prognosis as a pure serous adenocarcinoma. Also, serous carcinomas confined to an endometrial polyp behaved aggressively, with myometrial invasion and peritoneal spread.2
♥ Two major types of endometrial carcinomas exist: type I and type II.
♥ Serous carcinoma is the prototype for type II endometrial carcinomas -- these tumors usually occur in post-menopausal women without a history of hyperestrogenism. These neoplasms are aggressive and carry a poor prognosis.
♥ Endometrioid endometrial adenocarcinoma is the prototype for type I endometrial carcinomas -- these tumors usually occur in pre or peri-menopausal women with a history of hyperestrogenism. These neoplasms have a predictable pattern of spread and carry a better prognosis compared to type II endometrial carcinomas.
• Fallopian Tube : Papillary Serous Adenocarcinoma
1 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 248-9.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 662-4.
3 Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2482-3.
4 Boruta DM, Gehrig PA, Fader AN et al. Management of women with uterine papillary serous cancer: a Society of Gynecologic Oncology (SGO) review. Gynecol Oncol. 2009 Oct;115(1):142-53.
5 Slomovitz BM et al. Uterine papillary serous carcinoma (UPSC): a single institution review of 129 cases. Gynecol Oncol. 2003 Dec;91(3):463-9.