
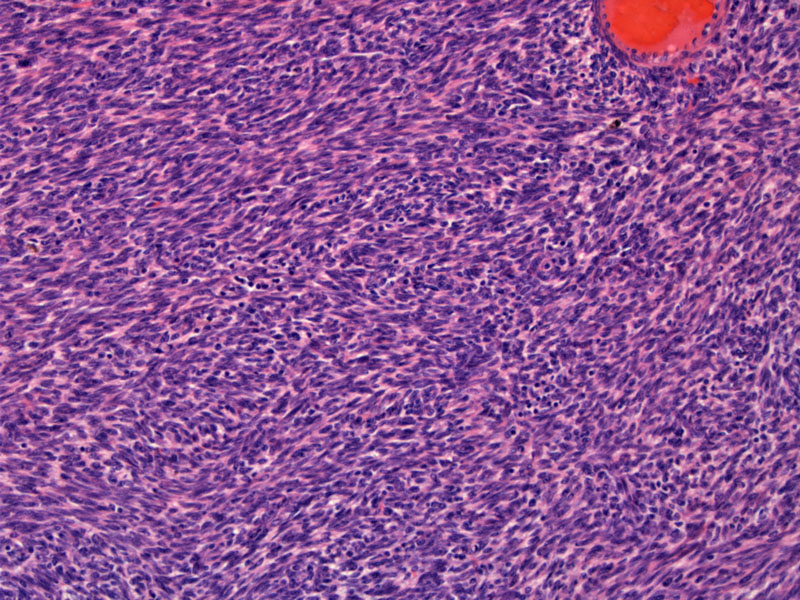
Highly cellular smooth muscle fascicles are arranged in a herringbone (basket-weave) pattern.
Thick-walled vessels are characteristic of this entity, in contrast with thin-walled and arborizing vessels in an endometrial stromal sarcoma (the main differential diagnostic consideration).
This is an entirely different case but looks remarkably similar. Note the prominent herringbone pattern.
Thick walled vessels are prominent. This helps identify the lesion.
The vessels have a noticeable eosinophilic encasement.
In the event of a negative CD10, the possibility of endometrial stromal sarcoma is significantly lessened. In most instances, ESS is CD10 positive whereas highly cellular leiomyomas are CD10 negative.
Staining for desmin should be strong and diffuse as seen here. But beware, some cases of endometrial stromal sarcoma, however, have demonstrated reactivity for desmin4 .
The WHO definition of a cellular leiomyoma is a leiomyoma that is 'significantly more cellular' than leiomyomas of the usual type. This definition leaves much to subjective interpretation, however, since most pathologists see an abundance of conventional leiomyomas, it is probably not difficult to surmise that a leiomyoma is more cellular than usual. Cellular leiomyomas exhibit much of the same features as conventional leiomyomas such as bland cytology, mitotic activity less than 5 mf/10 hpf and circumscription.1
Highly cellular leiomyomas, as the name implies, is even more cellular than cellular leiomyomas. The cellularity rivals that of an endometrial stromal neoplasm, and in fact, the main clinical significance of this entity is to separate highly cellular leiomyomas from endometrial stromal tumors (members include endometrial stromal nodule, endometrial stroma sarcoma and undifferentiated endometrial sarcoma). All of these neoplasms are spindled cellular proliferations in the myometrium, however, leiomyomas are benign and endometrial stroma sarcomas have malignant potential.2
In a study of endometrial mesenchymal tumors, Jung and colleagues found that 11 of 12 low-grade endometrial stromal sarcomas were immunoreactive for beta-catenin (nuclear staining) whereas none of the 9 uterine cellular leiomyomas stained with beta-catenin. Thus, nuclear beta-catenin may be a useful tool in distinguishing between these two entities.3
CD10 can also be a helpful IHC stain as it is usually positive in endometrial sarcoma and rarely positive in highly cellular leiomyomas.4
Benign and excision is curative; however, must distinguish from endometrial stromal sarcoma which is a malignant entity.
• Myometrium : Leiomyoma, Mitotically Active
• Myometrium : Benign Stromal Nodule
• Myometrium : Endometrial Stromal Sarcoma, Low-Grade
• Myometrium : Undifferentiated endometrial sarcoma
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 683-4.
2 Mills SE, ed. Sternberg's Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2515-6.
3 Jung CK, Jung JH, Lee A et al. Diagnostic use of nuclear beta-catenin expression for the assessment of endometrial stromal tumors. Mod Pathol. 2008 Jun;21(6):756-63.
4 Chu PG, Arber DA, Weiss LM, Chang KL. Utility of CD10 in distinguishing between endometrial stromal sarcoma and uterine smooth muscle tumors: an immunohistochemical comparison of 34 cases. Mod Pathol. 2001 May;14(5):465-71.