
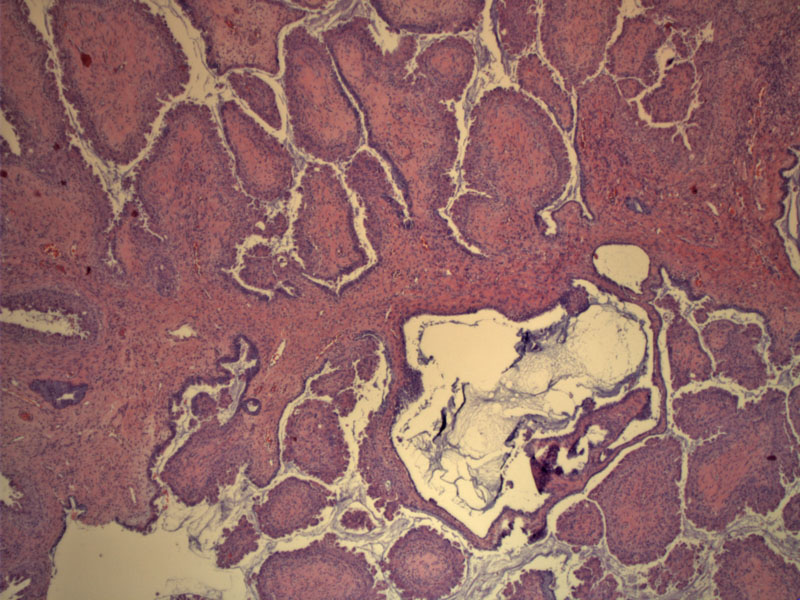
This neoplasm arose in a 60 year old woman as an adnexal mass with a complex papillary architecture. Broad branching papillae and mucin can be appreciated.
Bulbous papillae contain prominent fibrovascular cores; some have markedly edematous stroma.
The papillae are lined by endocervical-type epithelium with bluish mucin and so-called indifferent cells with abundant eosinophilic cytoplasm. There is no cytologic atypia; many cases of endocervical-type borderline tumors have adjacent areas of mucinous cystadenoma.
When not seen en face, you can appreciate how long and slender some of the papillae are. The cells lining the papillae have abundant eosinophilic cytoplasm (indifferent cells) and some demonstrate hobnail morphology (nuclei protruding into the interpapillary space).
Papillae are lined by columnar mucinous epithelial cells that resembled endocervical epithelium. Eosinophilic polygonal cells exhibit stratification and tufting, features also commonly found in serous borderline tumors.
Yet another low power image demonstrates papillary structures lined by endocervical-type mucinous epithelium and indifferent cells with tufting.
Mild nuclear atypia is present here. Also, note the acute inflammatory infiltrate in the stroma, a highly characteristic feature in this tumor type.
Indifferent cells line the papillae on top and mucinous endocervical-type cells line the papillae on the bottom. Some mild pleomorphism can be appreciated in the epithelial cells.
A higher power shows cells with oval mildly enlarged nuclei. Cellular budding can be appreciated.
Borderline mucinous tumors are traditionally divided into two categories: intestinal-type and endocervical-type. The intestinal-type is far more common and comprises approximately 85% of mucinous borderline tumors. The remaining 15% are of the endocervical-type and our knowledge of this entity is currently evolving.
Briefly, to compare and contrast intestinal-type and endocervical types: endocervical-type mucinous borderline tumors are smaller (average of 11 cm), more frequently bilateral (26%), whereas intestinal-types are larger (average 18-20 cm), rarely bilateral (6-8%). Furthermore endocervical types are strongly associated with endometriosis (31%) and endosalpingiosis (41%). Grossly, endocervical-types consist of one or just a few locules with intracystic papillae, whereas intestinal-types tend to be multilocated without grossly evident papillae. Microscopically, intestinal-type tumors exhibit a glandular and cystic architecture, whereas endocervical-types exhibit a complex papillary structure. Intestinal-types contain goblet and/or Paneth cells, which are absent in endocervical-types.1,2
The microscopic features of endocervical-type mucinous borderline tumors (EMBT) are as follows: (1) Marked resemblance to a serous borderline tumor with complex papillary structures; (2) Papillae are lined by a mixture of epithelial cell types such as columnar mucinous cells resembling endocervix, polygonal cells with abundant eosinophilic cytoplasm - the so called 'indifferent cells', ciliated cells resembling tubal epithelium, hobnail cells, endometrioid-type epithelium and squamoid cells; (3) an acute inflammatory infiltrate is frequently present in the stroma.
A note on confusing terminology: Some authors designate tumors consisting solely of endocervical-type epithelium and indifferent cells 'mucinous borderline tumors of the endocervical type' and those with a mixture of cell types are called 'endocervical-type mucinous border tumors of mixed cell types'. However, a recent study of 54 EMBT (Shappell) has revealed that most of these tumors are of a mixed cell type, therefore, Shappell and colleagues champion the term 'seromucinous tumors' of the ovary to emphasize their mixed histology and presence of both serous and mucinous features.
In general, these tumors have an excellent prognosis. Current evidence shows that microinvasion and intraepithelial carcinoma does not adversely affect prognosis. In a study of 31 EMBTs (Rodriguez), 21 patients who had long-term followup were alive at 5.7 years, including the 6 patients who exhibited microinvasion and/or intraepithelial carcinoma.
A similar study of 54 EMBTs (Shappell) confirmed that microinvasion and intraepithelial carcinoma, in addition to histologic features of cytologic atypia, necrosis or high mitotic activity, did not impact survival. The Shappell study, however, identified 7 cases of invasive carcinoma (defined as stromal invasion beyond 5 mm in diameter OR micropapillary architecture greater than 5 mm in diameter) in which two patients died of their disease. Thus, the authors conclude that frank invasion and/or micropapillary architecture are poor prognostic features.
• Ovary : Mucinous Borderline Tumor, Endocervical-type (Case 2)
• Ovary : Mucinous Borderline Tumor, Intestinal-type
1 Rodriguez IM, Irving JA, Prat J. Endocervical-like mucinous borderline tumors of the ovary: a clinicopathologic analysis of 31 cases. Am J Surg Pathol. 2004 Oct;28(10):1311-8.
2 Shappell HW, Riopel MA, Smith Sehdev AE et al. Diagnostic criteria and behavior of ovarian seromucinous (endocervical-type mucinous and mixed cell-type) tumors: atypical proliferative (borderline) tumors, intraepithelial, microinvasive, and invasive carcinomas. Am J Surg Pathol. 2002 Dec;26(12):1529-41.