
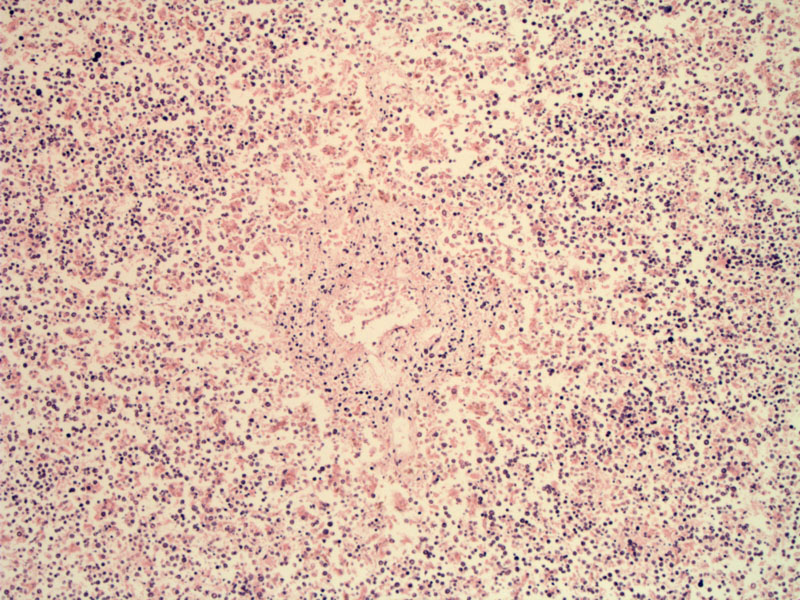
At low power, the placenta is hydropic (edematous). Due to the faded nature of the slide, it is difficult to see the architecture of the villi, but there is a vessel in the center of the image.
Inclusion bodies with a central clear to eosinophilic area and peripheral chromatin condensation (so-called ‘Lantern cells’) in erythroid precursor cell nuclei of the fetal vascular component.
Parvovirus B19, a small single-stranded DNA virus, is a potent inhibitor of erythropoiesis, due to its cytotoxicity to erythroid progenitor cells. The risk of adverse fetal outcome is increased if infection occurs during the first two trimesters of pregnancy but may also happen during the third trimester. Transmission from mother to fetus occurs in one-third of women with an acute infection, and serious fetal disease occurs in approximately 10% of these cases.1 Serious complications include fetal anemia, neurological anomalies, hydrops fetalis and fetal demise. Viral cardiac tropism can cause fetal myocarditis and aggravate the cardiac failure.
Note that Parvovirus B19 also causes aplastic crisis in sickle cell patients as well as erythema infectiosum (Fifth Disease) in hematologically normal children. This virus has a special affinity (tropism) for human erythroid progenitor cells and requires the P blood antigen receptor located to enter and infect the cell. Thus, very rare individuals lacking the P antigen are immune to parvovirus B19.2
Grossly, the placenta is enlarged, pale and hydropic (in fetal hydrops). Microscopically, ground-glass intranuclear inclusion bodies composed of viral particles can be identified in nucleated red blood cells. The inclusions are clear or lightly stained and the infected RBCs are sometimes called "lantern cells" because they reminded a pathologist of rotund Chinese lanterns.1
Parvovirus B19 is a widespread infection affects up to 1-5% of pregnant women, mainly with normal pregnancy outcome. Testing maternal serum for IgM antibodies against parvovirus B19 and DNA detection by PCR can confirm maternal infection.
Cordocentesis can allow for precise assessment of fetal anemia and transfusion as needed. Timely intrauterine transfusion of fetuses with severe hydrops fetalis reduces the risk of fetal death.
1 Baergen RN. Manual of Benirschke and Kaufmann's Pathology of the Human Placenta. New York, NY: Springer; 2005: 303-4.
2
Cennimo DJ, Dieudonne A. Parvovirus B19 Infection: eMedicine. Last updated August 4 2009. Available at: http://emedicine.medscape.com/article/961063-overview
Slides courtesy of Dr. Nancy Joste, Dept of Pathology at University of New Mexico, Albuquerque NM.