
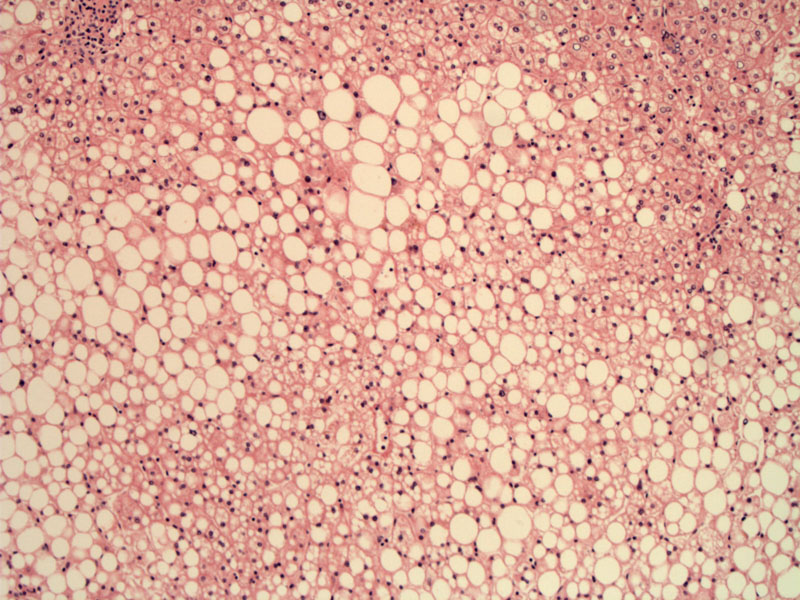
Macrovesicular steatosis is clearly evident at low power.
The fat droplet displaces the nuclei to the periphery of the hepatocyte. Note that although the neutrophilic infiltrate and Mallory hyaline may be more prominent in alcoholic hepatitis, many morphologic features of NASH and alcoholic hepatitis (as well as liver injury from drugs such as amiodarone) overlap, therefore, clinical history is critical at arriving at the proper diagnosis.
Fatty change in the liver is not always necessarily a result of alcohol consumption, although that is probably the most common etiology. Steatosis can be seen as a result of certain drugs, Reye syndrome, acute fatty liver of pregnancy and nonalcoholic fatty liver disease (NASH).
Fatty liver change can occur after just modest consumption of alcohol. Initially, small lipid drop droplets (microvesicular) are seen in the hepatocytes -- with increased alcohol intake, larger fat droplets are seen (macrovesicular) which push the hepatocyte nucleus to the periphery of the cell (Kumar).
In alcoholic liver disease, there are 3 stages. Fatty change is the initial histopathologic finding and this condition is reversible if the patient abstains from alcohol. If alcohol consumption continues, alcoholic steatohepatitis (with inflammation, hepatocyte swelling and necrosis, Mallory hyalin and fibrosis) may ensue, which may or may not be reversible. The end-stage may result in cirrhosis, which is not reversible.
Nonalcoholic fatty liver disease (NAFL) has similar, if not identical, features to alcoholic liver disease. NAFL is also subdivided into three categories: (1) largely asymptomatic accumulation of fat droplets (microvesicular or macrovesicular) within hepatocytes; (2) nonalcoholic steatohepatitis, also called NASH, which demonstrates steatosis, inflammation, Mallory bodies, ballooning degeneration, apoptosis and sinusoidal fibrosis -- basically the same features as alcoholic hepatitis; and (3) cirrhosis, estimated to occur in 10-30% of patients with NAFL. Many cases of 'idiopathic cirrhosis' are now attributed to NAFL, and there is no evidence that NAFL may also be synergistic with other liver diseases such as hepatitis C -- however, the contribution of NAFL to hepatocellular carcinoma is unknown at this time (Kumar, Iacobuzio)
Microvesicular versus macrovesicular steatosis:
Although microvesicular (multiple small lipid vacuoles within the hepatocyte) is seen in alcoholic and NAFL, the picture is generally that of macrovesicular steatosis, with a large lipid vacuole within the hepatocyte. Macrovesicular steatosis is more common and reversible. Some experts noted that microvesicular steatosis connotes a more severe pathologic process, seen in acute fatty liver of pregnancy, Reye syndrome, ingestion of antiviral agents (ie. HAART), tetracycline toxicity and valproic acid toxicity (Burt, Lefkowitch).
Alcoholic fatty liver disease is due to alcohol consumption and NAFL (nonalcoholic fatty liver diseas} which is linked with obesity, insulin resistance, hyperlipidemia and type II diabetes. Lab results usually demonstrate mildly to moderately elevated LFTs (ALT > AST -- in contrast to alcoholic hepatitis, where AST > ALT).
NAFL is more common in women and can be seen in obese children as well. A fatty liver may be demonstrated on imaging such as ultrasound or CT.
Burt AD, Mutton A, Day CP. Diagnosis and interpretation of steatosis and steatohepatitis. Semin Diagn Pathol 1998;15(4):246-58.
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 907-8.
Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 573-5.
Lefkowitch JH. Anatomic Pathology Board Review. Philadelphia, PA: Elvesier; 2006: 161.