
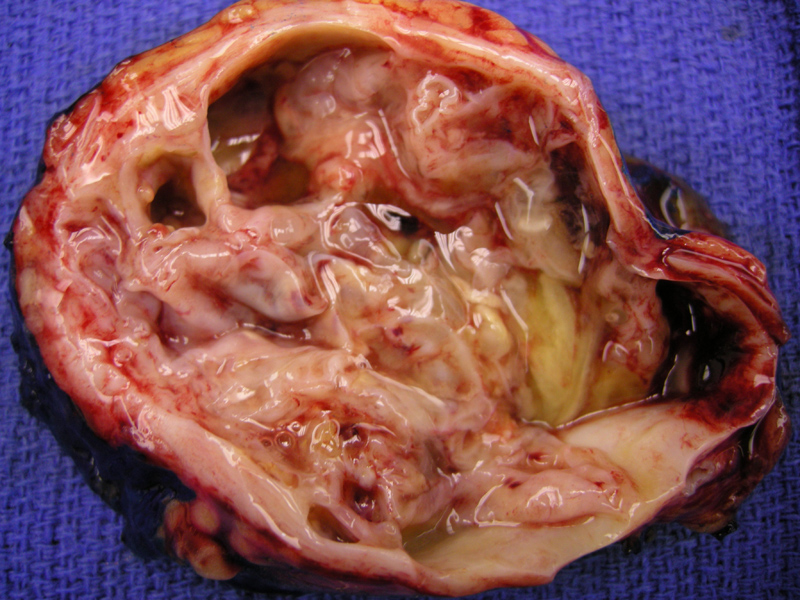
A mucinous cystic neoplasm showing a relatively smooth and shiny inner lining with some element of loculation. Note the thick pseudocapule.
A simple low columnar cyst lining is appreciated with underlying condensed spindled stroma indicative of ovarian-type stroma. This hormonely sensitive stroma expresses progesterone receptors, estrogen receptors, and inhibin. Compressed normal acini are seen underneath. Cysts do not communicate with the pancreatic ductal system.
Close inspection is often required to elucidate the intracytoplasmic mucin, seen as a faint blue tinge along the apical portion of some of the cells. The epithelium is usually columnar with apical mucin, but some cases can contain intestinal type epithelium with goblet cells and even Paneth cells may be present. While the epithelium here is uniformly bland, mucinous cystic neoplasms have the potential wide range of cytologic and architectural atypia, with prominent papillary proliferations with cribriform architecture and marked cytologic atypia. Note that atypia is often patchy and extensive sampling is required to exclude higher grade areas.
Mucinous cystic neoplasms are composed epithelial-lined cysts that produce mucin. Curiously, they exhibit an ovarian-type stroma and similar to ovarian epithelial tumors. Mucinous cystic neoplasms are graded as adenomas, borderine or carcinoma-in-situ depending on the degree of architectural and cytologic atypia. Cystadenocarcinomas demonstrate an invasive component.1,2
Mucinous cystic neoplasms are seen almost exclusively in perimenopausal female patients, although male cases have been well-documented. The M:F ratio is 1:9 with a mean age at diagnosis in the 5th decade.2 The neoplasm is most often located in the tail of the pancreas. Mucinous cystic neoplasms are almost always macrocystic, surrounded by a thick fibrotic capsule, elaborate tenacious mucin in some of the cysts, and do not communicate with the pancreatic ductal system.1,2
This is in contrast to intraductal papillary mucinous neoplasms, which are seen predominantly in the head of the pancreas, arise in older men (60–70 years), and involve the pancreatic ducts. It is also important to distinguish between serous cystic neoplasms, which are benign entities, and mucinous cystic neoplasms, which may be malignant and invasive.1,2
Seen almost exclusively in perimenopausal females, with mean age of diagnosis in the 50s.1,3 They usually arise in the tail or body of the gland.
Surgical resection.
Cured if there is no invasive component and surgically resected. Prognosis is significantlly worse if there is an invasive component, with a 5 year surivival rate of 50%.2
Φ Mucinous cystic neoplasms are comprised of epithelial cells that produce mucin, an ovarian-type stroma, arise in the tail of the pancreas and do not communicate with pancreatic ducts.
Φ Occurs almost exclusively in perimenopausal women.
Φ Mucinous cystic neoplasms can be graded as adenomas, borderline, carcinoma-in-situ or invasive.
Φ Must be distiniguished from serous cystic neoplasms which are benign.
Φ In contrast to mucinous cystic neoplasms, intraductal papillary mucinous neoplasms affect older men, communicate with the pancreatic ducts, more commonly involve the head of the gland and do not exhibit ovarian stroma.
• Pancreas : Mucinous Cystic Neoplasm with Moderate to High Grade Dypsplasia
• Pancreas : Intraductal Papillary Mucinous Neoplasm
1 Johns Hopkins Pancreas Cancer web.
Available at http://pathology2.jhu.edu/pancreascyst/index.cfm Last accessed on Sept 5th, 2010.
2 Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 487-490.
3 Volkan Adsay N. Cystic lesions of the pancreas. Mod Pathol. 2007 Feb;20 Suppl 1:S71-93.