
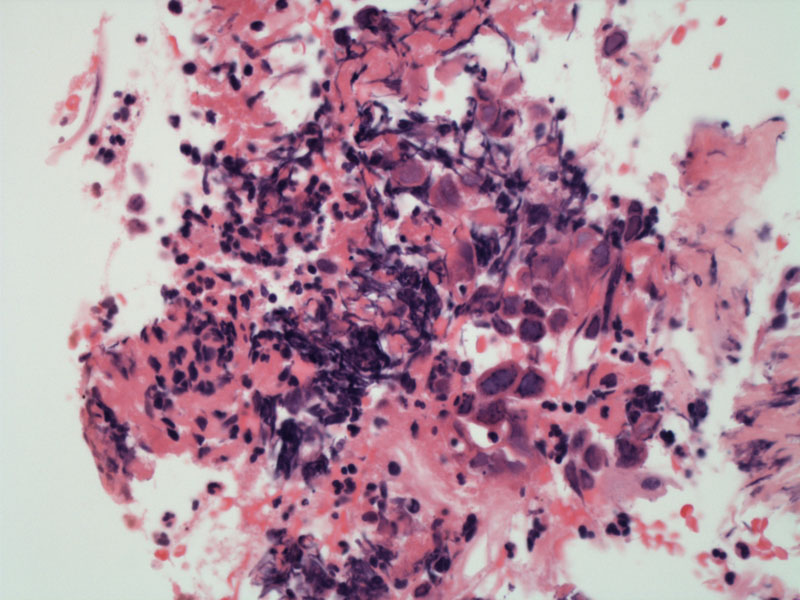
Keratinocyte necrosis is marked, but scattered intact cells are admixed in the neutrophilic debris.
Herpes cytopathic effect shows nuclear chromatin margination and nuclear molding in the acantholytic keratinocytes.
Herpetic stomatitis shows severe ulceration with epidermal necrosis.
Herpes gingivostomatitis is caused by herpes simplex virus type one and is usually transmitted via contact with saliva, although it can be spread by sexual contact or transplacentally as well. The prevalence of HSV-1 increases with age and can reach as high as 70-80% in the late adult years. Seroprevalence is also higher in groups of low socioeconomic status. There are two age-related peaks in the presentation of primary gingivostomatitis. The first is during childhood (between 6 months and 5 years) and the second is in the early twenties. There are varying degrees in severity of initial presentation and, when mild, can even be overlooked or mistaken for symptoms of teething.
Following an incubation period of several days to weeks, the patient usually begins to have non-specific symptoms such as malaise and myalgias. One to three days later, mucocutaneous vesicular eruptions appear on the tongue, lips, gingivae, buccal mucosa, and the hard and soft palates. These small 1-2 mm blisters then coalesce to form shallow, painful, irregular ulcers with a yellowish pseudomembrane and surrounded by an erythematous halo. Gingival features during a primary infection include diffuse, boggy swelling of the free and, at times, the attached gingivae. During this phase of the infection other features that may be present include: pyrexia, lethargy, loss of appetite, hypersalivation, headache, cutaneous rash and bilateral cervical lymphadenopathy. Many times associated pain from the infection can cause dysphagia to such a degree as to necessitate hospitalization for rehydration.
Many patients with primary gingivostomatitis may not require specific treatment other than pain control, however, according to published data, the recommended viral treatment is acyclovir (suspension or tablets) 200mg by mouth 5 times a day for 7 days. When given in the early phase of the infection, the severity may be decreased.
The ulcers of gingivostomatitis gradually heal over 10-14 days without scarring.
1. Arduino PG, Porter SR. Oral and Perioral Herpes simplex virus type 1 (HSV-1) infection. Overview of its management. Oral Dis 2006; 12:254-70
2. Kameyama T, Sujaku C, Yamamoto S, Hwang CBC, Shilitoe EJ. Shedding of herpes virus type 1 into saliva. J Oral Pathol 1988; 17:478-81
3. Scull C. Orofacial herpes simplex virus infections: current concepts in epidemiology, pathogenesis and treatment, and disorders in which the virus may be implicated. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1989; 68:701-10
4. Chavin PJ, Ajar AH. Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management. J Can Dent Assoc 2002; 68: 247-51
5. Huber MA. Herpes simplex type-1 virus infections. Quintessence Int 2003; 34: 453-67