
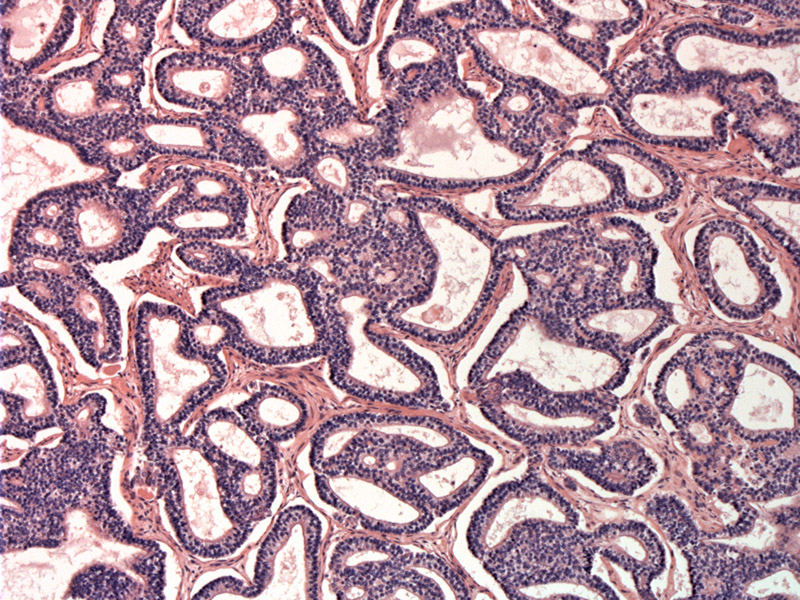
Closely-packed well-formed glands are seen. These irregularly branching tubular structures are lined with pseudostratified nonciliated columnar epithelium.
Squamous morules protrude partially into the glandular lumen. Note that there is only low grade cytological atypia.
A single layer of columnar epithelium with supranuclear vacuoles containing glycogen, almost like endometrial glands. There is a pauci-cellular stroma consisting of a loose network of bland mature fibroblast-like spindle cells
Branching glands with scant intervening stroma comprise the majority of this tumor. Note that there are some squamoid areas with more abundant eosinophilic cytoplasm.
This area shows the same glands but there is an admixture of malignant mesenchymal cells. This area makes is a biphasic example.
Pulmonary blastoma (PB) is a biphasic tumor with epithelial and mesenchymal components with two main histologic types: (1) predominantly epithelial or monophasic and (2) epithelial and mesenchymal or biphasic. Note that monophasic tumors are also known as well-differentiated fetal adenocarcinoma or adenocarcinoma of fetal lung type since these tumors resemble developing lung (during 9-11 weeks gestation).
The most current WHO classification lists fetal adenocarcinoma (ie. monophasic pulmonary blastoma) under the broader category of adenocarcinoma and biphasic pulmonary blastoma under the category of sarcomatoid tumors. Some authors (Fletcher) prefer to place both the monophasic and biphasic pulmonary blastoma under the category of "biphasic epithelial/mesenchymal neoplasms" since they are in effect the same entity along a continuum. Yes, very confusing, but take it up with the experts!
Grossly, the tumor is a solitary nodule with circumscribed borders, located in the mid-lung or periphery with size ranging from 1 to 20 cm. The cut surface is solid and white-yellow; hemorrhage and necrosis can occur in larger masses. Invasion into the visceral pleura is uncommon.
Microscopically in monophasic PB, branching and variably shaped glands are lined by columnar cells with clear cytoplasm and subnuclear vacuoles, lending an appearance similar to post-ovulatory endometrial glands. Within the glands, there may be morules, which are collections of oval or spindle cells with a squamoid appearance. Neither the glandular cells or morular cells exhibit much cytologic atypia. The intervening stroma in the monophasic tumor is bland and spindled. In biphasic PB, the glandular component is the same, but the meschenchymal component exhibits a sarcomatous appearance with blastema and rarely, bone, cartilage and mulinucleated trophoblast-like giant cells may be present.h
Affects adults in the third and fourth decades (mean age of diagnosis 35). Tumors can involve the bronchi leading to cough and hemotysis and those that arise in the periphery may remain asymptomatic. 80% of patients have a smoking history.
In contrast, pleuropulmonary blastoma affects primarily children and adolescents and the epithelial glandular component described above in pulmonary blastoma is not a prominent feature.
Complete surgical excision.
Monophasic pulmonary blastoma (aka well-differentiated fetal adenocarcinoma) are relatively indolent tumors, and most present at Stage I. Tumor-associated mortality approximately 10% (Zander). Biphasic tumors have considerably worse prognosis (Fletcher).
Pulmonary blastoma is a biphasic tumor with epithelial and mesenchymal elements.
The epithelial elements recapitulate lung development the fetus, but they also resemble endometrial glands with subnuclear vacuoles.
Monophasic pulmonary blastoma is also known as well-differentiated fetal adenocarcoma. Biphasic pulmonary blastoma is not classified under other names.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 193.
Zander DS, Farver CF. Pulmonary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2008: 587-590, 594-595.