
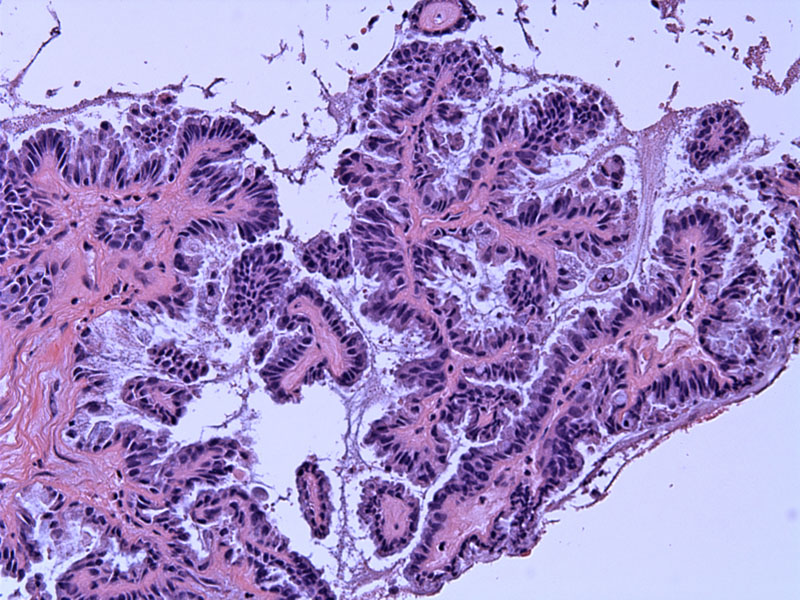
A main feature of borderline serous tumors are hierarchical branching papillae. Think of a tree branch with progressively smaller branches.
Another image of complex branching papillae without stromal invasion. Off to the far right, the gland embedded in the pink stroma are a tangential cut rather than invasion.
The lining cells are stratified, with mild to moderate cellular atypia and low mitotic activity. The lining cells may not be as clearly ciliated as the benign version. Detached cellular buds (tufting) are also another feature of this tumor.
Peritoneal washings demonstrate clusters of atypical serous cells.
The cell block obtained from the washing provides another view of detached serous cells.
The sloughed cells are negative for calretinin, thus ruling out a mesothelial origin. Note the single positively stained background mesothelial cell.
However, they are strongly positive for keratin 7, corroborating an epithelial origin.
ER positivity is present in the tumor cells.
Here is a gross image of a bosselated borderline tumor with external surface papillary excrescences.
This is another tumor with nodules of papillary aggregates located in the cyst lining.
Calcifications are common and can be found in the stroma and epithelium.
Calcifications can be quite extensive and cause a gritty feel on gross examination.
Variably sclerotic papillae can be seen in this serous borderline tumor.
This S-LMP tumor demonstrated ovarian endosalpingiosis. Note the center scalloped gland lined by fallopian tube epithelium. It is important not to overcall endosalpingiosis (a common finding in S-LMP) as invasive implants or malignant glands.
Serous borderline tumors (also known as serous tumors of low malignant potential, S-LMP) are currently one of most complex and intensely researched topics in gynecologic pathology. S-LMP encompass a heterogenous group of tumors, most of which are indolent actors but a significant minority do progress into carcinoma and eventually lead to the demise of the patient. We are challenged with the task of separating out this subgroup of women who may need closer monitoring and perhaps more aggressive treatment. What characteristics do these particular S-LMPs exhibit? Can we predict tumor behavior using a specified constellation of features?
Several key histologic features have been investigated, some of which demonstrate prognostic significance. It is beyond the scope of this website to discuss the finer details of these features, but we will point out some of the highlights.1-3
- Stromal microinvasion: clusters or nests of serous cells invade into the stromal, but by no more than 3 mm in depth. Generally considered a benign finding, but recent studies have demonstrated otherwise. Microinvasion may indicate a more aggressive tumor.
- Implants: Peritoneal or omental implants are classified into two categories: non-invasive (epithelial and desmoplastic) and invasive implants. Only invasive implants have been traditionally regarded as a poor prognostic factor. Newer studies question this assertion, as patients with non-invasive implants also have disease recurrence and eventual demise if followed over a long period of time.
- Lymph node involvement: In advanced borderline tumors, tumor may be present in pelvic or para-aortic lymph nodes. Two main patterns are seen: a papillary pattern that recapitulates the primary tumor and single or small nests of tumor. Generally considered not to impact survival.
- Micropapillary/cribrifrom architecture: This pattern is associated with a higher likelihood of bilaterality, surface papillary involvement and invasive implants.
The key feature separating borderline serous tumors from serous carcinoma is stromal invasion. By definition, borderline serous tumors do not exhibit stromal invasion (microinvasion will be discussed elsewhere). However, as mentioned above, borderline tumors may still behave in a most 'malignant' fashion, spreading viscerally through implants and via lymph nodes.
Borderline serous tumors occur slightly earlier than serous carcinoma (mean of 45 vs. 60 years, respectively).1 Most cases are asymptomatic, but may present with abdominal pain, abdominal enlargement and fullness, and elevated CA125.
Grossly, the neoplasms have cystic and solid areas with papillary excrescences in the cyst lining. Approximately half the tumors will exhibit papillary excrescences on the external surface of the ovary. 35-40% of cases are bilateral. Peritoneal or omental implants are found in 15-30% of cases.
Treatment is with surgical excision.
Over the long term, many patients do experience recurrences and require serial debulkings with adhesion formation until complete resection becomes impossible.
♣ Papillary structures lined by ciliated or columnar cells are key microscopic features.
♣ The serous lining is often tufted and pseudostratified. Cells often detach and slough off.
• Ovary : Serous Cystadenofibroma
• Ovary : Serous Borderline Tumor, Micropapillary Type
• Ovary : Serous Cystadenofibroma
• Ovary : Serous Borderline Tumor with Invasive Implants
• Ovary : Serous Borderline Tumor with Non-invasive Implants
• Ovary : Serous Carcinoma, Low Grade
• Ovary : Serous Adenocarcinoma, High Grade Papillary
1 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 398-406.
2 Kurman RJ, Seidman JD, Shih IM. Serous borderline tumours of the ovary. Histopathology. 2005 Sep;47(3):310-5.
3 Longacre TA, McKenney JK, Tazelaar HD et al. Ovarian Serous Tumors of Low Malignant Potential (Borderline TUmors): Outcome-Based Study of 276 Patients with Long-Term Followup. Am J Surg Pathol 200;29:707-723.