
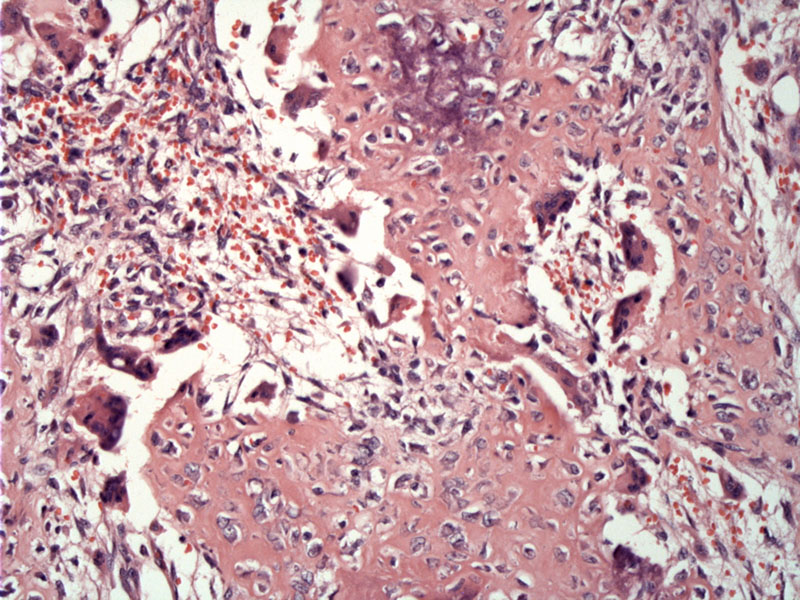
Loose fibroblastic tissue with immature bony trabeculae are heavily lined with osteoblasts. A highly vascularized connective tissue is typical, with stroma containing widely dilated capillaries (not seen here), and sometimes large dilated blood sinusoids may be present.
Prominent osteoblastic rimming is characteristic.
The prominent osteoblastic rimming is obvious as is the irregularity of interconnecting trabeculae and/or less mature osteoid.
Osteoblastoma (giant osteoid osteoma) is a bone-forming tumor composed of neoplastic osteoblasts that elaborate trabecular woven bone. It can arise in any bone, but the most common locations include the posterior spine (32%), femur (12%), tibia (10%) and foot/ankle (9%)(Folpe). It can be found within the cortex, medullary, or periosteal tissues.
On imaging, the lesion is round and often radiodense. By definition, it is greater than 2cm (as compared to 1-2cm for osteoid osteoma). Grossly, the appearance is red and granular with cystic change and hemorrhagic. The tumor is often surrounded by sclerotic bone.
Histologically, the tumor consists of haphazard interconnecting trabeculae rimmed by osteoblasts. The osteoblasts are round/ovoid with eccentric nuclei and moderate amounts of purple cytoplasm. The intertrabecular spaces contain connective tissue and delicate vessels. Scattered osteoclasts are present.
Several variants exist including cystic (large cystic change), cartilaginous (areas of hyaline or chondro-osseous cartilage), pseudomalignant (stromal cells exhibit degenerate atypia) and aggressive forms. The aggressive variant is controversial. Some authors do not believe that it is a separate entity. Microscopically, it is composed of enlarged osteoblasts with an epithelioid appearance, with abundant cytoplasm and vesicular nuclei. It is locally aggressive, but does not metastasize (Folpe, Fletcher).
The most important entity to rule out is an osteosarcoma (lack of osteoblastic rimming, infiltrative growth pattern, brisk mitotic activity with atypical forms and cytologic pleomorphism).
Occurs in any age group but in particular those in the 2nd through 4th decades of life. More common in males (3:1). Usually presents with local pain and a tender mass may be palpable. The clinical presentation and imaging can appear aggressive and elicit concern for malignancy.
Curettage is the most common treatment and recurrence is about 10% to 20% (Folpe).
Benign although there is some debate regarding the so-called aggressive variant. Malignant transformation is extraordinarily uncommon.
→Essentially identical to osteoid osteoma except for larger size (>2cm).
→Interconnecting trabeculae of bone rimmed by osteoblasts. Intertrabecular areas contain loose connective tissue and thin-walled vessels.
• Osseous : Conventional Osteosarcoma, High Grade
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1614-5.
Folpe AL, Inwards CY. Bone and Soft Tissue Pathology: Foundations in Diagnostic Pathology Philadelphia, PA: Elsevier; 2010: 316-320.
